Issue 213 – 6 February 2025

| Welcome to Practice Connect, a fortnightly update for practice managers, principals, nurses and administration staff on relevant issues, upcoming events and education. |

MyMedicare Updates

MyMedicare Program Guidelines published on 6 January 2025 contain detailed information and guidance for practices, general practitioners and patients who wish to voluntarily register with the MyMedicare Program.
We encourage general practices to familiarise themselves with these guidelines.
The MyMedicare Program Guidelines provide further information regarding:
- The Services Australia Organisation Register; a streamlined practice registration tool connecting a general practice, GPs, patients, MBS claiming and incentives in the one central system. The guidelines describe how the Organisation Register supports MyMedicare and new, existing and future health programs.
- Aboriginal Community Controlled Services or Aboriginal Medical Services can register their organisation sites under a ‘Hub and Spoke’ Model, whereby practices operating under this model are considered as a singular organisation for the purposes of MyMedicare Registration.
- General Practice Accreditation requirements and exemptions. Note that accreditation exemptions for non-traditional practices are in effect until 30 June 2025.
- Provider Registration Requirements outlining which providers are eligible
- Patient Registration Requirements including patient eligibility, exemptions to MBS service requirements, and more on patient registration
- Patient Consent of MyMedicare
- Withdrawing from MyMedicare
- MBS Items linked to MyMedicare
- Incentive Programs Linked to MyMedicare
- My Health Record and MyMedicare
For support on MyMedicare and GPACI, please contact the Practice Assist Help Desk on 1800 2 ASSIST (1800 2 277 478) or 08 6278 7900 or via email practiceassist@wapha.org.au.
New Quality Improvement (QI) Toolkit for General Practice in Aged Care Incentive now available

The General Practice in Aged Care Incentive (GPACI) QI Toolkit provides practical resources and guidance to support planned, preventative care and enhance coordination with multidisciplinary teams to improve patient outcomes and care continuity.
Practices can utilise the toolkit to streamline their workflows, access a range of helpful resources, and implement continuous QI activities, ultimately fostering a patient-centred approach in aged care settings. This toolkit has been developed by PHN’s working together nationally through the PHN Cooperative, the National Improvement Network Collaborative and the National MyMedicare PHN Implementation Program.
Primary Sense detects significant spike in Pneumonia cases across WA
Primary Sense has become a valuable tool in the early detection and management of pneumonia cases across WA. With 518 general practices utilising this technology, health care providers are now better equipped to respond to health trends.
Recent data shows a significant increase in pneumonia cases in 2024, with a 93% rise compared to the previous year. Notably, the period from September to November saw a 182% increase in cases compared to the same time frame in 2023. These statistics highlight the importance of advanced monitoring systems like Primary Sense.
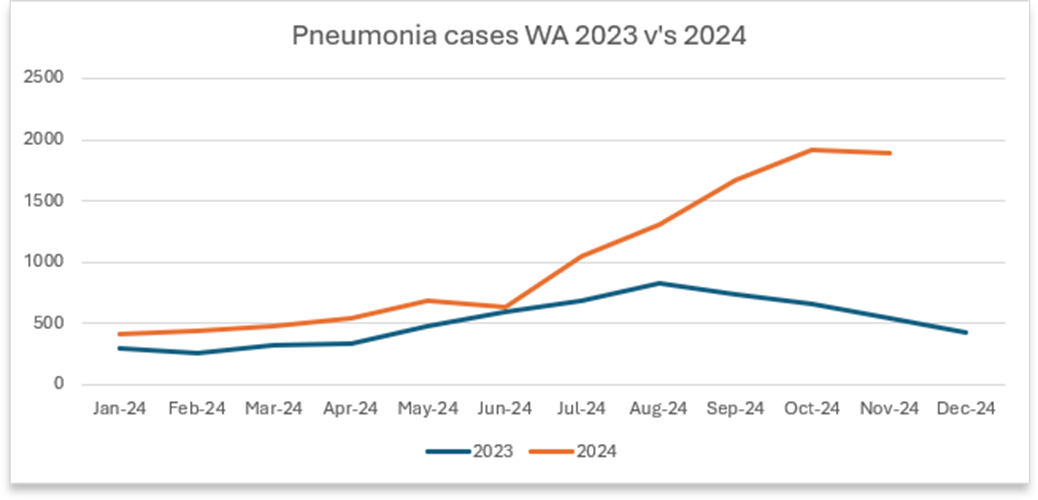
Primary Sense is a clinical decision support tool that extracts de-identified data from general practice records and provides real-time medication alerts, care prompts and reports during patient consultations. This continuous analysis helps clinical staff identify a patient’s complexity score, predict the risk of hospitalisation and make timely interventions to deliver appropriate care.
WA Primary Health Alliance (WAPHA) is playing a crucial role in embedding Primary Sense into practices and helping to optimise their use of data through the Primary Care Reporting Portal (PCRP). The PCRP is an encrypted platform that provides secure, on-demand, self-service access to real-time data reports for practices that share data with WAPHA via Primary Sense.
Looking ahead, WAPHA is planning to expand the reach and utilisation of Primary Sense by enhancing training and support for practices and ensuring that all health care providers can fully leverage the benefits of the data tool. There will also be a continued focus on analytics aimed at supporting the early detection of public health risks by monitoring primary care utilisation and identifying high-risk areas that require urgent attention.
For more information about Primary Sense, visit the Practice Assist Primary Sense webpage, call the Practice Assist help desk on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or email practiceassist@wapha.org.au
Virtual RACGP accredited QI activities for GPs using Primary Sense
Primary Sense reports can be used for clinical audits, identifying priority populations, proactive population health interventions and ensuring quality improvement (QI) activities have a data-driven approach that aligns with the Quintuple Aim for Health Care Improvement.
RACGP Member GPs who are interested in completing structured clinical audits using Primary Sense reports can register for the following virtual RACGP CPD accredited QI activities:
- 15 CPD hours: Optimising health outcomes for chronic obstructive pulmonary disorder patients with high complexity. For more information, visit RACGP MyCPD Activity ID: 904213 (COPD).
- 10 CPD hours: Optimising screening for chronic kidney disease in patients with diabetes using Primary Sense reports. For more information, visit RACGP MyCPD Activity ID: 849834 (CKD).
If you would like assistance with planning your QI activities, reach out to your local WAPHA Practice QI Coach by emailing QI@wapha.org.au or download the QI templates from the Practice Assist QI Tool Kit webpage.
Have you heard about the Skills in Demand (SID) visa?

The 482 temporary skill shortage (TSS) visa has been replaced by the Skills in Demand (SID) visa. Here are some key differences you may find useful if you are in the process of or thinking about employing an overseas health professional to your practice.
- The biggest change is the visa processing times. While the 482 TSS suggested a three month processing time, the new SID visa promotes a much quicker seven to 21 day turnaround (depending on which occupation list your health professional is classified under).
- Another important change benefitting the employee is the greater flexibility in finding a new employer sponsor if the original employment ends. Visa holders now have 180 days to find a new place of practice should the need arise.
- The new SID visa only requires one year of relevant work experience in the last five years, reduced from two years previously required on the 482 TSS.
- Permanent residency options are still available after two years of employment in Australia in the same occupation, however the SID allows for that employment to be with multiple employers, rather than the same employer rule under the 482 TSS.
There are further changes anticipated, which may be positive for rural employers. Keep in touch with the Rural Health West Workforce Solutions team for further updates and reach out if you have any visa-related questions recruit@ruralhealthwest.com.au
Seniors Information Resource now available

The Seniors Information Resource is a new information resource which helps Western Australian seniors navigate a wide range of state-wide services and concessions.
The Seniors Information Resource is an action of the State Seniors Strategy 2023-2033 and was developed in response to feedback from older people across Western Australia who identified the need for clear, accessible information about services, programs and concessions available to them.
It includes information about housing, health, aged care services, elder abuse, technology and communication, transport, connecting with community, end of life planning and a range of other topics. It aims to increase awareness and uptake of existing services, concessions and programs for older people in Western Australia.
A limited number are available at local governments, libraries, Community Resource Centres, the WA Seniors Card Perth office and seniors’ services across Western Australia.
You can download the Seniors Information Resource here.
Additionally, a website for the Resource is currently in development and is scheduled for release in 2025.
If you would like to express interest in ordering a limited number of hardcopies (minimum of 50 copies, maximum of 100 copies) or provide feedback on the Resource, please contact the Department of Communities’ Seniors and Ageing team on 1800 176 888 or email seniors@communities.wa.gov.au.
All feedback will be considered for the development of a new Seniors Information Resource website and the next edition of the hardcopy resource, both scheduled for release in 2025.
WA Virtual Emergency Department Update – Bunbury expansion
Since its launch in September 2023, the WA Virtual Emergency Department (WAVED) has been progressively expanded to give more patients the option of having a virtual consultation with a specialist emergency physician in the comfort of their own home.
Currently, WAVED accepts referrals for adult patients from St John WA (SJWA) and a small number of additional agreed referrers in the Perth metropolitan area. In partnership with SJWA, WAVED will expand into the Greater Bunbury area from late February 2025. Eligible patients referred by SJWA (either before or after ambulance dispatch) will be assessed via a telehealth platform, providing earlier access to emergency specialist assessment. Where appropriate, care will be delivered in the community including referral to other appropriate services and supports. Transfer to a physical emergency department will still occur where this is likely to benefit the patient.
It is important that GPs are aware of this service, as WAVED clinicians may make direct contact to discuss a patient’s care and involve the GP in decision-making. All relevant clinical information is documented in a discharge summary which is securely transmitted to the nominated GP and uploaded to the patient’s My Health Record.
Expansion of WAVED will continue throughout 2025, with an initial focus on developing a referral pathway from the HealthDirect advice line and establishing a paediatric sub-service.
Find out more here.
Have you heard about the free perinatal mental health services offered by PANDA?
This February PANDA is asking Health Professionals to share information about PANDAs services, so that they can work together to better support expecting and new parents.
PANDA provides free counselling and support for expecting and new parents with a child up to the age of 12 months. They support all parents, especially those facing barriers accessing mainstream services. They have articles and a mental health checklist translated into 40 languages and free printed brochures can be sent to your service through our online portal.
PANDA also provides free education and resources for health care providers who support the mental health and wellbeing of families. Their interactive online courses cover the core knowledge and skills related to perinatal mental health, conditions, and associated risks.
They also offer secondary consultation for healthcare professionals, where our clinicians provide counselling and support to you if you’re experiencing challenges in your role.
More information available here.

2025 WA RSV Infant and Maternal Immunisation Program

RSV is a highly infectious virus that is the most common cause of respiratory infections in children, with almost all children being infected at least once in their first 2 years of life. Following the successful implementation of the 2024 Respiratory Syncytial Virus (RSV) Infant Immunisation Program, WA Health will offer a 2025 WA RSV Infant and Maternal Immunisation Program to continue protecting infants from severe RSV disease.
Option A – Abrysvo: From 3 February 2025, pregnant women will be able to receive Abrysvo vaccine year-round for free under the National Immunisation Program (NIP) between 28-36 weeks of pregnancy.
Option B – Beyfortus® (Nirsevimab): From 1 April to 30 September 2025, some infants will be eligible to receive a dose of Beyfortus® under the state-funded infant RSV immunisation program, under the following eligibility cohorts:
- infants born between 1 October 2024 to 30 September 2025 whose mother did not receive Abrysvo
- Aboriginal infants and children born on or after 1 October 2023
- infants with specific high risk medical conditions (MRC) born on or after 1 October 2023.
Information on the 2025 WA RSV Infant and Maternal Immunisation Program, as well as more information regarding eligibility is available here.
The WA Immunisation Schedule and WA Aboriginal Immunisation Schedule have been updated to include Abrysvo, and will be updated to include Beyfortus® closer to the program start date.
Providers can view the WA Health 2025 WA Respiratory Syncytial Virus (RSV) Infant and Maternal Immunisation Program webpage for provider information.
Please see here for Commonwealth resources and information regarding the Abrysvo vaccine for eligible pregnant women.
Protect pregnant patients and their infants

Healthcare provider recommendation is a key facilitator for antenatal vaccine uptake, increasing the likelihood of acceptance by 10-12 times compared to those who do not receive a recommendation. Maternal vaccines are provided free under the National Immunisation Program schedule.
Pertussis
|
Respiratory Syncytial Virus (RSV)
|
Influenza
You may like to refer to SKAI for resources to assist with vaccine counselling. |
Changes to the AIR “Vaccine type” field
A new bespoke antenatal indictor was added to the Australian Immunisation Register (AIR) in early December 2024, allowing vaccination providers to report to AIR if a person is pregnant at the time of vaccine administration.
On 9 February 2025, vaccination providers using the AIR site will be able to report to the AIR:
- the new antenatal indicator
- the following options under the Vaccine type field: NIP/Commonwealth & other.
The collection of antenatal data ensures that the AIR contains a complete and reliable dataset to enable the monitoring of:
- immunisation coverage and administration
- the effectiveness and safety of maternal vaccines and vaccination programs.
These enhancements are being implemented in a phased approach; vaccination providers wanting to know when these changes will be available in their clinical software are encouraged to speak with their software provider.
See here for further information.
Pertussis Clinical Newsletters
The Immunisation Coalition have created two 15-minute clinical newsletters raising awareness of whooping cough (pertussis), vaccination options for maternal vaccination, children under 5 years and in adolescence as per the National Immunisation Program, and to also consider vaccinating adults who are in close contact with infants and young children, to further reduce the risk of catching whooping cough during outbreaks.
Newsletter learning objectives:
- Summarise the epidemiology and burden of pertussis, including its transmission and infection process, and potential complications, particularly in young infants
- Identify the signs and symptoms of pertussis and its clinical impact in infants and children
- Apply diagnostic methods for pertussis, including laboratory tests and clinical criteria
- Summarise the importance of vaccinating specific populations against pertussis
- Explain the importance of vaccination in preventing pertussis and the current recommendations for DTPa and dTpa vaccines
- Summarise the treatment options for pertussis, including the role of antibiotics and supportive care
- Outline strategies that healthcare professionals can consider that reduce the spread of pertussis during outbreaks
Access the newsletters here.
Meningococcal Disease Update
Presented by Immunisation Coalition
19 February 2025 (3pm to 4pm AWST)
The Immunisation Coalition are presenting a disease update on Invasive Meningococcal Disease.
On completion of this educational activity, attendees will be able to:
- Review the epidemiology of Invasive Meningococcal Disease (IMD) in Australia
- Identify the serotypes causing IMD and presentation trends according to the National Notifiable Diseases Surveillance System
- Describe who is eligible for free Meningococcal ACWY and B on the NIP schedule
- Describe the impact of vaccination practices on IMD rates if other States followed a MenB free vaccination program, additional to the current NIP schedule.
To register and for further information, click here.

World Cancer Day 2025 – Is your practice integrated with the National Cancer Screening Register (NCSR)?

This year, we observed World Cancer Day on Tuesday 4 February.
WA Primary Health Alliance recommends all practices regularly check and participate in training about current screening guidelines for breast, cervical and bowel cancer. The easiest and best way to do this is integration with NCSR.
Clinicians can access their patients’ cancer screening information and submit program forms directly to the NCSR through their practice’s clinical software. Learn more about the NCSR and its benefits on their website.
Practices using Medical Director or Best Practice can integrate their systems to access a patient’s bowel and cervical screening records directly within the patient record.
Incorporating the NCSR into your practice helps to:
- provide a history of screening results to better track patients’ past screening outcomes
- ensure timely participation in screening programs by sending patients reminders
- provide a safety net for at-risk individuals so practices are best placed to follow-up and care for their patients who need it most
For further information regarding integration, click here.
Cervical Screening Webinar
The National Cervical Screening Program Guidelines for the management of screen-detected abnormalities, screening in specific populations and investigation of abnormal vaginal bleeding have now been updated to incorporate and support best clinical practice.
The new Guidelines are now live and are available at: Cervical Cancer Screening Guidelines | Cancer Council
Please note the changes will not go live in the National Cancer Screening Register (NCSR) until April 2025.
Discretion and best clinical judgement are to be used regarding the use and ‘compliance’ with the Guidelines during this time.
The new program Guidelines are supported with the following healthcare provider training:

2025 cervical screening update: what you need to know about the latest clinical guidelines
RACGP Specific Interests, in partnership with the Commonwealth Department of Health and Aged Care and the National Cervical Screening Program (NCSP), is presenting a webinar to educate health professionals on the latest update to the National Cervical Screening Program Guidelines.
It is being presented by:
- Dr Lara Roeske, Provost, RACGP Specific Interests and member of the NCSP Self-collection Implementation Committee
- Prof Deborah Bateson, Professor of Practice at the Daffodil Centre, clinician researcher with a focus on the elimination of cervical cancer in Australia and the Pacific.
The education is aimed at general practitioners, but all health professionals will benefit from this education.
As a key stakeholder in health promotion and education, we would appreciate if you can assist in communicating the details of this webinar to your members.
The education will be held twice:
- Tuesday 11 February – Register here
- Thursday 13 March – Register here
If you have any questions or concerns, please feel free to contact us via NCSPcommittees@health.gov.au

Helpful resources for diagnosing and treating Long COVID-19
The Australian Government is giving $1.1 million to the National Health and Medical Research Council (NHMRC) to create new clinical guidelines for Long COVID.
These guidelines aim to help doctors diagnose and treat Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and related chronic conditions.
The goal is to improve treatments, coping strategies, and care options for patients.
The following resources support clinicians in diagnosing and managing ME/CFS and Long-COVID, and are available now:
- Book: Long COVID by Prof. Steven Faux (2024) – endorsed by former Chief Medical Officer Professor Paul Kelly.
- Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (Bmj, 2024)
- National PASC Plan | Australian Government DoHAC (2024)
- Managing Post-COVID Symptoms for Patients (RACGP, 2023)
- Caring for Adult Patients with Post-COVID-19 Conditions (RACGP, 2021)
- ME/CFS diagnosis and Management Guidelines (NICE, 2021)
- HealthDirect: Long-COVID and ME/CFS
Onboarding and Offboarding for the National COVID-19 Vaccine Program
From 2 January 2025, the Department of Health and Aged Care Vaccination Operation Centre (VOC) will be the main point of contact for matters relating to the National COVID-19 Vaccine Program (NCVP) for primary care providers.>
PHNs, including WA Primary Health Alliance, will no longer have responsibility for provider onboarding, offboarding and dealing with queries regarding the NCVP. This change is part of the planned transition of COVID-19 activities to align with other Australian Government funded vaccine programs.
New sites wishing to onboard onto the National COVID-19 Vaccine Program (NCVP) will now need to contact VOC directly to register their expression of interest.
Existing sites wishing to offboard will also be required to contact VOC directly to finalise their participation in the Program.
Queries related to the NCVP should also be directed to VOC from this date.
Any new, recommencing or offboarding sites should contact VOC at COVID19VaccineOperationsCentre@health.gov.au or by telephone at 1800 318 208.

New Resources for Electronic Prescribing, Active Script Lists and Cyber Security
The Australian Digital Health Agency has added a suite of new self-paced RACGP, ACRRM and AAPM CPD accredited online learning modules for electronic prescriptions and cyber security.
Learn how electronic prescribing and the token system saves time, improves medicine safety through mitigating transcription errors, and reduces the number of lost or misplaced scripts, as well as how to set this up in your practice. Active Script Lists provide a token management solution, enabling patients or their authorised representative to view and manage all their ePrescription tokens in the same place without the need to keep track of multiple SMS or email tokens. Patients can now access their Active Script List through the my health app, or at a registered dispensing pharmacy.
With the new cyber security modules, all members of the practice team can be confident that they are prioritising patient safety when using online conferencing and telehealth technologies, or when working from home!
These modules sit alongside a suite of other resources supporting primary care providers to implement and use digital health tools including My Health Record, for efficient, connected and patient-centred care.



Telehealth Clinical Skills Program
Presented by Australian College of Rural and Remote Medicine (ACRRM)
Online Module & Interactive Workshop
The Australian College of Rural and Remote Medicine (ACRRM) offers a comprehensive online course to equip medical practitioners with best-practice telehealth consultation skills.
Program Overview:
- Online Module: Self-paced learning with videos and reading materials (approx.
4.5 hours). - Interactive Workshop: A live 90-minute session, featuring expert-led role plays and
Q&A.
Key Features:

- Earn 6 CPD hours.
- Learn from experienced FACRRMs in telehealth across diverse clinical settings.
- Covers consultation setup, physical assessments, legal aspects, and the use of adjunctive devices in virtual care.
Register now for a Clinician Assist WA live demonstration
Presented by Clinician Assist WA
Multiple Times & Dates Online

Clinician Assist WA is a secure website providing GPs and other health professionals with guidance for assessing, managing and referring patients across Western Australia. It has replaced HealthPathways WA, offering the same trusted local guidance, features and functionality and remains available at no cost.
The Clinician Assist WA team will run online demonstrations facilitated by a GP Clinical Editor throughout 2025 to support users. These sessions will demonstrate how to maximise integration of Clinician Assist WA into your clinical practice. Learn key functionalities of the website and how to access condition specific tools and resources, Referral Access Criteria (RAC) (where available), GPbook Specialist Directory and visiting specialist rosters.
Sessions have been approved for 1 CPD Educational Hour with RACGP and will be held online on the following dates:
- Wednesday 12 March 2025 – 12:30pm to 1:15pm
- Thursday 12 June 2025 – 12:30pm to 1:15pm
- Wednesday 17 September 2025 – 12:30pm to 1:15pm
- Tuesday 18 November 2025 – 12:30pm to 1:15pm
Demonstrations are open to general practitioners, general practice staff and other health professionals registered to practice in WA.
Paid GP online training: IAR-DST to guide mental health referrals – February and March training dates
Presented by WA Primary Health Alliance
Multiple Dates & Times
WA Primary Health Alliance (WAPHA) is providing GPs in WA with paid online Initial Assessment and Referral Decision Support Tool (IAR-DST) training, designed to help practitioners and clinicians recommend the most appropriate level of care for a person seeking mental health support.
GPs and GP registrars who attend the two workshops will be remunerated $300 and CPD hours are available.
For the latest IAR-DST training dates and registration links, visit the WAPHA IAR-DST webpage.
ADAPT Australia – Educational Event on Drug Allergy & Penicillin Allergy Testing (CPD Opportunity)
Presented by The University of Western Australia
29 March 2025 (Harry Perkins Institute of Medical Research, Nedlands)
The University of Western Australia invite doctors and nurses to participate in ADAPT Australia, an educational event designed to enhance your knowledge and confidence in drug allergy and penicillin allergy testing. There is no prior experience of allergy testing necessary. This event is part of a research trial aimed at assessing the validity and effectiveness of the educational materials provided.
Key Details:
- In-person sessions (preferred) and online options available for rural/remote participants or those with travel constraints.
- Participation in the event counts towards Continuing Professional Development (CPD).
- The course will cover critical aspects of drug allergy management and penicillin allergy testing, designed to improve your clinical practice.
More information and registration details here.
Clinical workshops for GPs in your area

The GP Management of Patient Depression and Suicidality course, developed by Rural Clinical School of WA general practitioners, in collaboration with Psychiatrist Dr Mat Coleman, is designed to enhance the skills of GP’s in treating depression and suicidality.
The program is made up of two modalities:
Part 1: Online Module – (approx. 90mins to complete all modules)
- Recognition and Assessment of Depression
- Interventions
- Suicidality, suicide risk assessment and prevention
- Groups requiring special consideration
- GP Wellbeing and supports
- Practice Resources, Clinical Practice Guidelines & local resources
Part 2: Face-to-Face Workshop – (approx. 90 mins with a light meal included)
Collaborative conversations, including sharing of clinical experiences, complex scenario analyses, debriefing and learning from adverse outcomes. Facilitated by a GP and supported by a local psychiatrist.
Both online module and workshop are CPD accredited.
Location and dates for each workshop will be displayed when you choose your preference within the registration form. Please note, if you are a rural GP and unable to attend your local workshop, you are welcome to register for a metro workshop.
- Rockingham – Wednesday 19 February
- Mandurah – Thursday 20 February
- Crawley – Wednesday 26 February
- Guildford – Thursday 27 February
- Joondalup – Wednesday 5 March
- Crawley – Thursday 6 March
- Guildford – Wednesday 12 March
- Joondalup – Thursday 13 March
- Mandurah – Wednesday 19 March
- Rockingham – Thursday 20 March
View the GP Management of Patient Depression and Suicidality page for more information.
Exploring VAD in practice – Health Professional Forum
Presented by South Metropolitan Health Service & WA Voluntary Assisted Dying Statewide Navigator Service
Friday 7 March 2025 (9.00am to 5.00pm The Hub, Bentley Technology Park, Bentley)
Join South Metropolitan Health Service and the WA Voluntary Assisted Dying Statewide Care Navigator Service for a day of shared learning, insights and updates in Voluntary Assisted Dying (VAD) relevant to health professionals caring for people exploring and accessing VAD in diverse settings.
This free event is catered and suitable for all health professionals, including:
- medical practitioners
- nurse practitioners
- nurses
- social workers
- those supporting people at the end of their lives.
WA Rural Health Conference 2025 – Registrations now open!
Presented by Rural Health West
22 & 23 March 2025
Mark your calendars for the WA Rural Health Conference, Pan Pacific Perth on Saturday 22 to Sunday 23 March 2025. Early bird registrations are now open!
This year’s theme, “Strengthening rural WA: One connection at a time,” brings together a diverse range of rural health professionals including:
- Aboriginal health workers and practitioners
- Allied health workers
- GPs, medical practitioners, and medical officers
- Health administrators
- Health organisations and stakeholders
- Health and medical students
- Medical registrars
- Nurses and midwives
The preliminary program is now available, which includes sessions that focus on collaboration, connection, and community impact.
For full details and to take advantage of early bird rates, please visit www.waruralhealthconference.com.au
For any inquiries, please contact the Events Team at warhc@ruralhealthwest.com.au or call 08 6389 4500.

Other Webinars, Events & Workshops
| WA HIV s100 Prescriber Update – Expression of Interest Presented by ASHM Online Course |
| BreastScreen WA visit to Pemberton Presented by BreastScreen WA 3 February to 17 February |
| BreastScreen WA visit to Boddington Presented by BreastScreen WA 4 February to 12 February |
| BreastScreen WA visit to Esperance Presented by BreastScreen WA 14 February to 17 March |
| BreastScreen WA visit to Fremantle Presented by BreastScreen WA 17 February to 26 February |
| HR – Recap of 2024 and Preview of 2025 Presented by AAPM 18 February |
| BreastScreen WA visit to Busselton Presented by BreastScreen WA 18 February to 11 July |
| BreastScreen WA visit to Gingin Presented by BreastScreen WA 24 February to 12 March |
| BreastScreen WA visit to Booragoon Presented by BreastScreen WA 27 February to 31 March |
| WA General Paediatric Update Day Presented by Perth Children’s Hospital – General Paediatrics 6 March |
| Course in Ear Wax Removal Presented by Benchmarque Group 12 March |
| Save the date: WA Rural Health Conference 2025 Presented by Rural Health West 22 March to 23 March |
| Talking About Suicide in Practice (3 hour interactive webinar) Presented by Black Dog Institute 29 March |
| Curing Hepatitis C in Primary Care Presented by ASHM 31 March |
| Integrating Digital Resources into Mental Health Care (2 hour interactive webinar) Presented by Black Dog Institute 7 April |
| Diabetes In-Depth health professional training Presented by Diabetes WA 15 April |
| Dealing with Depression in Rural Australia (Blended Learning) Presented by Black Dog Institute 11 May |
Acknowledgement
WA Primary Health Alliance acknowledges and pays respect to the Traditional Owners and Elders of this country and recognises the significant importance of their cultural heritage, values and beliefs and how these contribute to the positive health and wellbeing of the whole community.



