Issue 217 – 3 April 2025

| Welcome to Practice Connect, a fortnightly update for practice managers, principals, nurses and administration staff on relevant issues, upcoming events and education. |

Head to Health evolves to Medicare Mental Health

Head to Health has evolved to Medicare Mental Health, making face-to-face, digital and telephone initiatives more consistent with other trusted health services funded by the Australian Government.
Medicare Mental Health helps people access the mental health and wellbeing services that are right for them. It also makes it easier for GPs and other health professionals to support the mental health of the people they look after, and those who support them, through improving access to, and coordination of, mental health services in their local community.
Medicare Mental Health includes:
- A digital platform – The website includes evidence based digital mental health resources, apps and online programs. This includes dedicated online forums, peer support services, chat and email services.
- National phone service (1800 595 212) – Offers free confidential assessment and referral for anyone seeking help for their mental and emotional wellbeing and/or wanting to support a patient, or someone they care about.
- A network of Medicare Mental Health Centres – These services are free and confidential for people aged 18 and over. No referral, appointment or Medicare card is needed.
Using telehealth to support and manage a patient with complex care needs

View Street Medical in North Perth is using telehealth to support and manage a 60-year-old male patient with complex care needs, including chronic disease, chronic pain and fatigue. Dr Belinda Wozencroft explained that the patient requires monthly appointments to review and manage his condition because he also receives care from numerous specialists, however his pain and fatigue make it difficult for him to attend the practice without transport assistance.
“Using telehealth has greatly benefited the patient, allowing him to attend reviews from home, saving energy and reducing pain. Telehealth not only ensures regular engagement for medication management but also keeps his chronic disease management, recalls and referrals up to date. If he has physical concerns needing in-person evaluation, there is flexibility to switch to face-to-face appointments. Scheduled in-person reviews every four to six months allow for necessary health checks like blood pressure monitoring, ECGs and immunisation updates,” Dr Wozencroft said.
During the telehealth appointments, Dr Wozencroft uses dual screens to enable her to consult with the patient via videoconference, while accessing real-time documentation in the clinical software system to ensure that e-scripts, e-referrals and e-requests for pathology are promptly actioned.
“The use of telehealth has become an indispensable tool in this patient’s health care, making his complex care needs easier to manage by enabling more efficient and convenient access to care. The ability to use videoconferencing means consultations can be billed to MBS for mental health plans, GP management plans and reviews when appropriate,” Dr Wozencroft said.
For further information and resources about using telehealth in your practice, visit the Practice Assist Digital Health Tool Kit webpage, call the Practice Assist help desk on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or email practiceassist@wapha.org.au
Ensure you receive fast payments for the services you deliver to veterans
Did you know that the Department of Veterans Affairs (DVA) funds tens of thousands of client health services each year?
Health service claims submitted via DVA’s Webclaim that are correct, and meet all DVA requirements, are usually paid on the same day or within a few business days.
A common issue of claims being submitted incorrectly is the omission of the client’s condition on the claim or a discrepancy between the condition specified and the client’s DVA accepted condition (583 rejection reason).
This rejection is easy to resolve – simply confirm the correct condition and re-submit the claim
You can submit claims electronically via DVA Webclaim using the Health Professional Online Service (HPOS) portal through your Provider Digital Access (PRODA) account or via your practice software. Claims sent via mail are accepted; however, processing times are considerably longer. We therefore encourage electronic claiming for faster payments. More information on claiming can be found on the DVA website.
To query a claim rejection or to discuss electronic claiming options please contact provider.support@dva.gov.au for assistance.
Curtin Student-Led Physiotherapy Clinic
Looking for cost-effective musculoskeletal physiotherapy for your clients?
The Curtin Health and Wellness Centre provides affordable physiotherapy assessment and care for musculoskeletal conditions and is for everyone. Care is provided by physiotherapy students in their final years of study, and intermittently, post-graduate physiotherapy students. All consultations are closely supervised by experienced physiotherapists in our professional treatment areas.
The treatments offered are patient centred and evidence-guided.
The Clinic offers treatment for a variety of musculoskeletal conditions, including:
🤕 back pain
🤕 neck pain and headaches
🤕 sports injuries, such as sprains and strains
🤕 rehabilitation following surgery or injury
🤕 arthritis and joint pain

Clients can self-refer by calling 9266 1717. Medical practitioners or health professionals can also provide the Clinic with client details using the referral form.
To find out more about the Curtin Physiotherapy Clinic, including opening hours, visit the Physiotherapy Clinic website.

Update to the Modified Monash Model (MMM) classification system aims to increase Medicare support for some WA communities

The Australian Government Department of Health and Aged Care (DHAC) recently announced changes to the Distribution Priority Area (DPA) and Modified Monash Model (MMM) classifications. These changes will mean that some GPs and local communities could benefit from increased Medicare support through increased bulk billing rates or a wider pool of doctors to recruit from.
Distribution Priority Area (DPA) changes
The DPA classification identifies locations in Australia with a shortage of GP services. Areas classified as DPA are eligible for various initiatives aimed at increasing the supply of GPs, including the recruitment of International Medical Graduates (IMGs) who must work in a DPA to access Medicare benefits.
Full DPA status is automatically given to general practices located in MM 2-7.
On 10 March 2025, DHAC announced changes to the DPA classifications, with 17 localities being reclassified, nine of which are in WA. Notable changes include:
- Cockburn, Gosnells, and Mundaring-Swan View: These areas have been upgraded from non-DPA to full DPA status.
- Armadale, Byford, Kalamunda, and Swan: These areas have moved from partial DPA to full DPA status.
Modified Monash Model (MMM) Changes
The MMM classification system defines whether a location is metropolitan, rural, remote, or very remote. It uses a scale from MM 1 (major cities) to MM 7 (very remote areas). The MMM classification impacts the level of incentives available to GPs working in these areas.
Recent changes to the MMM classifications have seen two WA locations, Green Head and Leeman, reclassified from MM 5 (small rural towns) to MM 6 (remote communities). This reclassification allows these areas to access higher levels of federally funded programs and incentives.
Impact on General Practices in WA
Changes to DPA and MMM classifications will impact some GPs and local communities in WA:
- Increased Recruitment of GPs: The reclassification of areas to full DPA status makes them eligible to recruit IMGs, which can help address GP shortages in these regions.
- Enhanced Incentives: The reclassification of Green Head and Leeman to MM 6 means these areas can now access larger bulk billing incentives and other federally funded programs. This can make it more attractive for GPs to work in these remote communities.
The Health Workforce Locator now reflects changes to the DPA and MMM geographical classification systems. These updates will be implemented in Services Australia’s system on 13 April 2025, taking effect from that date.
Rural Health West: Navigating the DPA Changes
How the Five Year Scheme can support rural GP recruitment
Last month’s changes to the Distribution Priority Area (DPA) classifications have significant implications for rural general practice recruitment, particularly in Western Australia. While the DPA updates reflect the latest Census and workforce data, the reality is that they will make it harder for some rural and remote communities to recruit International Medical Graduates (IMGs), a key part of the rural health workforce.
At Rural Health West, we understand the concerns of rural practices that rely on IMGs to deliver essential healthcare. Although these changes present challenges, we want to reassure rural practices that there are alternative pathways to recruit and retain IMGs in WA – particularly through the Five Year International Medical Graduate Recruitment Scheme (Five Year Scheme).
The Five Year Scheme: A critical lever for rural GP recruitment
The Five Year Scheme remains a powerful incentive to attract IMGs to work in rural and remote areas. In essence, the Scheme reduces the 10-year moratorium placed on IMG access to Medicare provider numbers for those working in rural areas. IMGs working in remote and very remote locations can have their moratorium significantly shortened under the Scheme.
The Scheme aims to:
- Provide incentives to attract appropriately qualified and experienced IMGs to meet current and future community needs.
- Increase the supply of skilled IMGs in rural and remote Australia.
- Enhance the professional development, skills, and knowledge of IMGs in Australia.
- Bring greater stability to the provision of GP services in rural and remote communities.
Crucially, Rural Health West has some discretion in determining locations for the Five Year Scheme, allowing us to respond to emerging workforce gaps. This flexibility means we can continue supporting practices that may now find it harder to recruit under the revised DPA classifications.
What does this mean for rural practices?
DPA status affects which locations are eligible to access certain workforce programs and recruit IMGs. The Five Year Scheme is only available to IMGs working in rural and remote locations. This means rural practices still have viable options to secure much-needed doctors.
Kelli Porter, General Manager Workforce at Rural Health West, explains:
“The broader application of DPA is undoubtedly a challenge, but we have tools to work around them. The Five Year Scheme remains a great incentive for IMGs to establish a career in rural WA. We can work closely with communities to ensure that rural practices remain supported in their recruitment efforts.”
“We understand how disruptive sudden classification changes can be, and our team is ready to assist practices in navigating these updates. The good news is that we can still place doctors in areas where they are most needed, ensuring continuity of care for rural communities.”
How Rural Health West can help
We encourage you to reach out to our experienced GP recruitment team to explore options under the Five Year Scheme. Our team can:
- Assess eligibility for the Five Year Scheme and help facilitate IMG placements.
- Advocate for appropriate workforce solutions based on community needs.
- Provide ongoing support and resources to ensure rural practices remain sustainable.
While we acknowledge the challenges these DPA changes bring, we remain committed
to ensuring rural WA continues to have a strong and stable GP workforce. By leveraging
the flexibility of the Five Year Scheme, we can continue to help communities secure the doctors they need.
If you’d like to discuss how Rural Health West can assist your practice, contact us today on recruit@ruralhealthwest.com.au

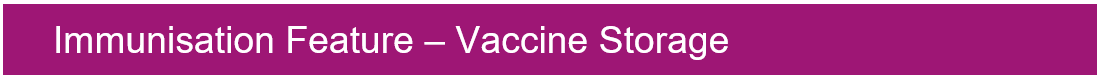
Tips for safe vaccine storage in your practice
Correct vaccine storage and handling has been an important factor in preventing and eradicating many common vaccine-preventable diseases.
Yet, each year, storage and handling errors result in revaccination of many patients and significant financial loss because of wasted vaccines.
Failure to store and handle vaccines properly can reduce vaccine potency, resulting in inadequate immune responses in patients and poor protection against disease.
Patients can lose confidence in vaccines and immunisation service providers if they have to be revaccinated after receiving vaccines that may have been compromised.
Below are some quick tips to ensure that your vaccine fridge and data logging remain compliant and your vaccines and patients are being protected.
Visit the WA Health Cold Chain Management page for further information on safe vaccine storage in your practice.

2025 WA Influenza Immunisation Program
The 2025 WA Influenza Immunisation program has now commenced.
Annual vaccination is the most important way to prevent influenza and its complications.
Influenza vaccination is recommended for all persons aged ≥6 months.
- All vaccinations must be recorded on the Australian Immunisation Register (AIR).
- The ‘vaccine type’ field should be used to record specific details of the vaccine administered, e.g. National Immunisation Program (NIP) or state funded (other).
- If a person had a 2024 formulation influenza vaccine in late 2024 or early 2025, they are still recommended to receive a 2025 formulation influenza vaccine.
Eligibility for government-funded influenza vaccines is listed on the WA Immunisation Schedule and the WA Aboriginal Immunisation Schedule.
To read the latest Vaccine Update regarding funded vaccines please see here.
Measles Alert
At least ten cases of measles have been confirmed in WA this year. An infectious diseases health alert was issued on Monday 31 March by the Department of Health.
Increasing Measles outbreaks have been noted globally and cases of measles in returned overseas travellers has increased across Australia, particularly amongst those returning from South and Southeast Asian Countries.
The incubation period for measles is on average around 10 days. Symptoms typically begin with fever, runny nose, cough, red eyes, and a sore throat. A few days later, a rash appears — usually starting on the face or neck, before spreading across the body. The rash generally lasts for up to a week.
Measles is highly infectious and can be transmitted via airborne droplets to those sharing the same airspace e.g. in waiting rooms and for 30 minutes after the case has left the room.
- Patients with a measles-compatible illness should be promptly identified at reception or triage, fitted with a surgical mask, and isolated in a separate room with the door shut (or negative pressure isolation room, where available).
- Only staff who are immune to measles (two documented doses of measles-containing vaccine, serological evidence of immunity; or born before 1966) should attend the patient.
- Use airborne transmission-based precautions when assessing the patient: wear a N95/P2 mask and eyewear in addition to standard precautions.
- Leave the examination room vacant for at least 30 minutes after the patient has left and ensure thorough surface and environmental cleaning and disinfection occurs.
- Urgently notify your local Public Health Unit of suspected measles by telephone, or 1800 434 122 (after hours on-call). Do not wait for laboratory confirmation before notifying a suspected case.
Anyone born after 1965 and planning overseas travel should ensure that they are immune to measles (have evidence of 2 doses of a measles containing vaccine) prior to travel.
- MMR vaccine should be given to those who are not immune, or unsure of their status.
- Infants can receive a dose of MMR from as young as 6 months of age if they are travelling to areas with a high risk for measles, after an individual risk assessment.
- Measles vaccination rates for 2-year-olds in WA has recently decreased to 91%; to achieve community immunity and prevent outbreaks, at least 95% of a population needs to be vaccinated.
Download Measles posters for display in practice
- Measles-poster—call-before-entering-or-use-mask.pdf
- Measles-poster—could-this-patient-have-measles—triage-for-EDs-GPs.pdf
To see the full Infectious Disease Health Alert, click here.
New AIR update on warning messages for flu and RSV vaccines
The National Centre for Immunisation Research and Surveillance (NCIRS) recently published an Australian Immunisation Register (AIR) Update on the introduction of age limit-related warning messages for some influenza and RSV vaccines when vaccinations are being reported to the AIR.
The latest in a series of short guides on how to use the AIR effectively, and improve the quality of AIR data, this update notes that immunisation providers will now receive a warning message (when using both software and the AIR site) if they attempt to report administration of Afluria Quad, Fluzone High-Dose Quad, Fluad Quad and Arexvy vaccines to the AIR for individuals who are under the recommended age limits for those vaccines.
To access the update, click here.
2025 RSV Beyfortus Infant Immunisation Program
The state funded component of the 2025 WA RSV Infant and Maternal Immunisation Program has now commenced. Beyfortus (nirsevimab) is free for eligible newborns and at-risk children across WA from 1 April through to 30 September 2025.
Some infants will be eligible to receive Beyfortus under the state-funded infant RSV immunisation program, under the following eligible cohorts:
- infants born between 1 October 2024 to 30 September 2025 whose mother did not receive Abrysvo
- Aboriginal infants and children born on or after 1 October 2023
- infants with specific high risk medical conditions (MRC) born on or after 1 October 2023
If a mother has received Abrysvo, Beyfortus is not recommended for the infant, unless the infant has a high-risk condition, the mother is immunocompromised or insufficient time (<2 weeks) between Abrysvo and the infant’s birth has occurred, to ensure adequate antibody generation.
This eligibility is applicable statewide except for in the Kimberley and Pilbara regions, where RSV immunisation is available to the above cohorts year-round, due to local RSV epidemiological trends.
To read the full Vaccine Update 421, including available education, ordering and cold chain advice, please click here.
Respiratory Syncytial Virus (RSV) update to the Sharing Knowledge About Immunisation (SKAI) website
The RSV vaccine is available for eligible pregnant women under the National Immunisation Program and is recommended between 28 to 36 weeks of pregnancy.
The SKAI website has been updated with webpages to support conversations between providers and pregnant women about RSV vaccination in pregnancy.
These webpages include:
- information about RSV disease and vaccine for pregnant women and their partners
- vaccination recommendations during the third trimester.
It’s important to inform your patients about the RSV vaccine. Find more RSV resources to support administration and conversations with your patients here.
Updated NCIRS resources on RSV, pharmacy vaccination
The National Centre for Immunisation Research and Surveillance (NCIRS) has recently updated the following resources:
| NCIRS’ RSV FAQs Six new questions and responses – including the RSV vaccine Abrysvo and the long-acting monoclonal antibody Beyfortus (nirsevimab) – have been added to this resource. |
| Co-administration of vaccines for adults The aim of this guide is to help immunisation providers identify vaccines that can be co-administered (i.e. given at the same visit) for adults. The visually refreshed resource includes new and updated guidance on co-administration of COVID-19, RSV, Japanese encephalitis and other vaccines as well as links to useful resources. |
| Vaccine recommendations for pregnant women – a guide for health professionals This resource has been revised to include additional detail on RSV and COVID-19 vaccines as well as information on maternal antibody transfer during the third trimester of pregnancy. |
ATAGI releases 2025 statement on COVID-19 vaccines
The Australian Technical Advisory Group on Immunisation (ATAGI) has released its annual statement on COVID-19 vaccination in Australia in 2025.
The statement notes that adults remain eligible for a COVID-19 vaccine every 12 months, while vaccination every six months is recommended for adults aged 75 years and over.
Two vaccines – Comirnaty JN.1 and Comirnaty Omicron XBB.1.5 – are available for use in Australia this year.
Although all adults are eligible for a COVID-19 vaccine every 12 months, the statement specifies differences in risk–benefit between those recommended and those eligible to receive COVID-19 vaccination.
COVID-19 vaccines remain funded for all recommended and eligible individuals, including those without a Medicare card.
To read the full statement, click here.

National Lung Cancer Screening Program Health Workforce Education Webinar
Presented by Lung Foundation Australia
Tuesday 15 April 2025 (4.00pm to 5.30pm AWST)

The National Lung Cancer Screening Program is designed to reduce lung cancer-related illness and death by encouraging high-risk individuals to take part in targeted routine screening. The program is an Australian Government initiative implemented by the Department of Health and Aged Care in partnership with Cancer Australia and the National Aboriginal Community Controlled Health Organisation.
Hear from the expert panel for an exclusive webinar hosted by Lung Foundation Australia on how to successfully integrate lung cancer screening into your everyday practice.
Topics include:
- National Lung Cancer Screening Program Overview
- Screening Pathway Overview
- Nodule Management
- National Cancer Screening Register
Ask the expert panel your questions at registration or live during the Q&A session!
The session will be available on-demand from the following day, please register now for access to the recording.
For further information and to register, click here.

Help improve our clinical and referral pathways
To ensure that Primary Health Network (PHN) led clinical and referral pathways platforms continue to be fit for purpose and meeting the evolving needs of GPs and their patients, WA Primary Health Alliance, on behalf of PHNs nationally, is seeking your valuable input on clinical and referral pathways platforms.
As part of the first two phases of the research component, the project has heard from a range of perspectives via in-depth interviews and survey responses, providing valuable insights which will inform the final report. This third and final research phase seeks to ensure that all GPs have the opportunity to provide their input and share their experiences.
Through this final survey, we are seeking to gather detailed quantitative survey responses from GPs, to gain deeper insights into individual experiences, attitudes and expectations as they relate to existing platforms and any potential future solutions.
Your participation will take less than 15 minutes and is greatly appreciated. Simply complete the anonymous survey linked here.
About the clinical and referral pathways project
This project aims to identify areas of improvement with the existing clinical referral pathways offerings to deliver better patient care within general practice. You can learn more about the project here.

Paediatric Sepsis Week 2025
Presented by Perth Children’s Hospital
Wednesday 16 April 2025 (11.30am to 1.30pm AWST Online only via Zoom)
Paediatric Sepsis Week is an international event dedicated to raising awareness of paediatric sepsis. Sepsis is a dysregulated host response to infection and a leading cause of morbidity and mortality. It affects each child differently, and post-sepsis recovery can have a significant impact on children and their families, highlighting the need for ongoing support.
The Perth Children’s Hospital (PCH) Sepsis Program has launched an Australian-first Sepsis Follow-Up Program to support children recovering from sepsis. This program includes nurse-led virtual health appointments at 3, 6, and 12 months, in collaboration with the PCH Infectious Diseases team. It also provides care coordination and connections with tertiary and primary health services. General practitioners will receive a letter informing them of their patient’s enrolment in the program.
As part of Paediatric Sepsis Week, they are promoting PCH’s sepsis resources and the Best Sepsis Care for Our Kids event.
Register here to join the event, and explore these Sepsis resources for further learning.


Immunisation – Winter Wellness Webinar
Presented by WA Primary Health Alliance
10 April 2025 (5pm to 6pm AWST)

The 2025 winter season is fast approaching.
Join us for this webinar to learn about the new immunisation schedules and which vaccines will be available for respiratory syncytial virus (RSV), influenza, pneumococcal and COVID-19.
GPs and vaccine service providers play a crucial role in ordering and administering vaccines, educating patients and ensuring coverage across all age groups.
This webinar will cover the following topics:
- Key successes of the 2024 infant RSV immunisation program as a vaccine service provider.
- Implementation strategies for the 2025 program.
- 2025 eligibility criteria for pregnant women and infants.
- 2025 influenza vaccines.
- JN.1 COVID-19 vaccine and the associated ATAGI guidelines.
This webinar is accredited for 1 RACGP EA CPD hour.
To find out more view the flyer here and register today.
If you can’t attend this webinar, there is an RACGP winter immunisation webinar on 29 April 2025 – click here for detail.
Paediatric Weight Management Event
Presented by Perth Children’s Hospital and WA Primary Health Alliance
3 May 2025 (9am to 4.15pm AWST) In Person

The Perth Children’s Hospital Healthy Weight Service and WA Primary Health Alliance invite GPs to a face-to-face event focused on effective weight management strategies.
This RACGP-accredited event will combine interactive learning with case study workshops, providing a well-rounded educational experience.
The following topics will be covered during the event:
- Raising the issue when weight is not the primary concern.
- The language of weight management.
- Goal setting with patients.
- Local opportunities, where to go for information and resources, and referring on.
- How to improve dietary intake.
- How to improve physical activity.
- Pharmacotherapy.
There are 50 places available for GPs at this event, which is accredited for 7 RACGP EA CPD hours.
To find out more, view the flyer and register today.
GP Telehealth Networking Event
Presented by WA Primary Health Alliance
8 May 2025 (6.30pm to 8.30pm AWST)
Join us for a relaxed panel discussion and networking event focused on the use of telehealth in primary care from different perspectives.
Using telehealth can significantly improve GP workload by streamlining workflows, improving efficiency and providing faster, more convenient patient care.
Offering telehealth services at your practice, in conjunction with standard face-to-face consults, expands primary care opportunities for you and your patients.
WA Primary Health Alliance is currently providing support to GPs who are interested in using telehealth within their practice or within a residential aged care home.
To find out more, view the flyer and register today.
Expressions of Interest
Shared Care Model: Healthy Weight Webinar
Presented by WA Primary Health Alliance and WA Country Health Service
20 May 2025 (6pm to 7.30pm AWST) MS Teams (online)
Currently, almost 1 in 4 children are overweight or obese and those with complex medical comorbidities are often referred to the Perth Children’s Hospital – Healthy Weight Service (PCH-HWS).
Regional referrals to the PCH-HWS represent 25% of all referrals and waitlists for this service are long and increasing.
To better address childhood obesity in regional areas, a shared model of care for managing children living in regional WA with high Body Mass Index (BMI) has been developed.
The key principles of the service delivery model include:
- Improving the equity of service provision for children across regional WA.
- Enhanced triage for appropriate support for obesity-related medical conditions.
- Providing obesity management support closer to home wherever possible.
The model will be rolled out in WA Country Health Service (WACHS) regions, using a phased approach throughout 2025.
WA Primary Health Alliance (WAPHA) and WA Country Health Service (WACHS) are hosting an information session for General Practitioners (GPs) to learn about the important role they can play in supporting children within the shared care model and hear from clinical and public health experts in the field, including Perth Children’s Hospital – Healthy Weight Service.
If you are a GP interested in the shared care model for managing children with overweight or obesity in regional WA, please register your interest. Registration is capped by region for equitable access and places are allocated on a first-come, first-served basis
Complete an Expression of Interest here in attending this event. Successful applicants will be notified and provided with link to event. Remuneration provided in accordance with WAPHA’s Paid Participation Policy.
Aboriginal cultural diversity training – free online training for all practice staff
Presented by WA Primary Health Alliance
Available until June 2025

To help improve health outcomes for Aboriginal people, WA Primary Health Alliance (WAPHA) is offering free online Aboriginal cultural diversity training for all general practice staff.
The free online training is the SBS Inclusion Program (First Nations) that includes short learning modules, which take approximately an hour to complete in total, with the following learning outcomes:
- Improving knowledge about the history of Aboriginal culture and experiences.
- Understanding how to identify myths versus facts. Comprehending some of the stereotypes and assumptions sometimes made about Aboriginal people.
- Recognising the importance of spirituality in Aboriginal culture.
- Recognising the importance of family and kinship in Aboriginal culture.
- Grasping the impact of colonisation on Aboriginal people.
- Comprehending the trauma felt by the Stolen Generations and the intergenerational trauma still being felt today.
- Implementing tools to actively participate in the reconciliation process as both an individual and a business.
- Explaining what the Uluru Statement from the Heart is and how it came about.
- Describing the events that led to the referendum in 2023, which proposed Aboriginal people be recognised in an enshrined Voice to Parliament.
To find out more view the flyer here and register today!
Register now for a Clinician Assist WA live demonstration
Presented by Clinician Assist WA
Multiple Times & Dates Online

Clinician Assist WA is a secure website providing GPs and other health professionals with guidance for assessing, managing and referring patients across Western Australia. It has replaced HealthPathways WA, offering the same trusted local guidance, features and functionality and remains available at no cost.
The Clinician Assist WA team will run online demonstrations facilitated by a GP Clinical Editor throughout 2025 to support users. These sessions will demonstrate how to maximise integration of Clinician Assist WA into your clinical practice. Learn key functionalities of the website and how to access condition specific tools and resources, Referral Access Criteria (RAC) (where available), GPbook Specialist Directory and visiting specialist rosters.
Sessions have been approved for 1 CPD Educational Hour with RACGP and will be held online on the following dates:
- Thursday 12 June 2025 – 12:30pm to 1:15pm
- Wednesday 17 September 2025 – 12:30pm to 1:15pm
- Tuesday 18 November 2025 – 12:30pm to 1:15pm
Demonstrations are open to general practitioners, general practice staff and other health professionals registered to practice in WA.
Other Webinars, Events & Workshops
Acknowledgement
WA Primary Health Alliance acknowledges and pays respect to the Traditional Owners and Elders of this country and recognises the significant importance of their cultural heritage, values and beliefs and how these contribute to the positive health and wellbeing of the whole community.