Issue 223 – 26 June 2025

| Welcome to Practice Connect, a fortnightly update for practice managers, principals, nurses and administration staff on relevant issues, upcoming events and education. |
New Chronic Condition Management details announced

MBS Online has recently published the Upcoming Changes to Chronic Disease Management Framework
confirming the new framework for chronic condition management from 1 July 2025.
The changes simplify, streamline, and modernise the arrangements for health care professionals and patients.
- Chronic Disease Management items 721, 723 and 732 will cease and be replaced by new item numbers and rebates for a streamlined single GP Chronic Condition Management Plan.
- Where multidisciplinary care is required, patients will be able to access the same range and number of services currently available via a standard referral letter, consistent with GP referrals to other medical specialties.
Further details can be found on MBS Online.
For support on MBS changes, please contact the Practice Assist Help Desk on 1800 2 ASSIST (1800 2 277 478) or 08 6278 7900 or via email practiceassist@wapha.org.au
What do Chronic Conditions Management changes mean for practice nurses, Aboriginal and Torres Strait Islander health practitioners and Aboriginal health workers?

MBS Online has recently published a new factsheet outlining what the upcoming Changes to Chronic Conditions Management (CCM) MBS items mean for other members of the general practice team that often play an important role in chronic condition management plans and ongoing care.
- Overall, these changes are intended to modernise, streamline and simplify the MBS items for patients with a chronic condition.
- The ability for practice nurses, Aboriginal and Torres Strait Islander Health Practitioners and Aboriginal Health Workers to assist in the preparation of a GPCCMP has been specified in the regulatory arrangements for the new items.
- The nature of the services that can be provided using items 10997, 93201, 93202,10950, 81300, 93000, 93013, 93048 and 93061 are not changing as part of these reforms. However, there are changes to the item descriptors for these items because of the removal of GPMPs and TCAs, and commencement of GPCCMPs. These changes:
- Allow patients that had a General Practitioner Management Plan (GPMP) and/or Team Care Arrangement (TCA) prior to 1 July 2025 to continue to access these services under those plans until 30 June 2027. See transition agreements factsheet.
- Allow patients that have had a GPCCMP prepared or reviewed in the previous 18 months to access these services.
- For services provided using MBS items 10950, 81300, 93000, 93013, 93048 and 93061, referrals written on or after 1 July 2025 will be in the form of a letter, not the form used previously. Referrals written before 1 July 2025 remain valid until all services under the referral have been provided. See separate factsheet on referral requirements.
For more information on CCM changes, MBS Online has released a selection of Factsheets here:
MBS Online – Upcoming changes to the MBS Chronic Disease Management Framework
For support on MyMedicare and upcoming CCM Changes, please contact Practice Assist help desk on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or email practiceassist@wapha.org.au
What do Chronic Conditions Management changes mean for Allied Health Providers?
Allied health professionals providing MBS services should be aware of the changes to plan and referral requirements.
Requirements for the GP or prescribed medical practitioner to collaborate with other members of the team when preparing or reviewing a patient’s plan have been removed. Patients will be referred directly to services. Allied health providers do not need to confirm their agreement to participate in the patient’s multidisciplinary team.
The nature of the individual and group allied health services that can be provided under the chronic condition management arrangements are not changing.
Transition arrangements will be in place for 2 years to ensure current patients do not lose access to services.
From 1 July 2025:
- GP Management Plans (GPMPs) and Team Care Arrangements (TCAs) will be replaced with a single GP Chronic Condition Management Plan (GPCCMP).
- Requirements for the GP or prescribed medical practitioner to collaborate with other members of the team when preparing or reviewing a patient’s plan have been removed. Patients will be referred directly to services. Allied health providers do not need to confirm their agreement to participate in the patient’s multidisciplinary team.
- Patients with a GPCCMP will be able to access individual allied health services, and for patients with type 2 diabetes only, group allied health services.
- Patients with a GPMP and/or TCA in place prior to 1 July 2025 can continue to access these services under those plans until 30 June 2027. Referrals written prior to 1 July 2025 remain valid until all services under the referral have been provided. See transition arrangements factsheet.
- Allied health providers should be aware that referrals for allied health services written on or after 1 July 2025 must meet the new referral requirements. See referral arrangements for allied health services factsheet.
- All other MBS requirements of the existing allied health services are unchanged, including requirements to provide written reports to the referring medical practitioner.
For more information, MBS Online has released a selection of Factsheets here:
MBS Online – Upcoming changes to the MBS Chronic Disease Management Framework
For support on MyMedicare and upcoming CCM Changes, please contact Practice Assist help desk on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or email practiceassist@wapha.org.au
Changes to MBS from 1 July 2025

From 1 July 2025, there will be changes to the Medicare Benefits Schedule (MBS). These changes include annual fee indexation and a range of administrative and policy changes to implement the government’s response to recommendations from the MBS Review Taskforce and the Medical Services Advisory Committee.
Changes also include:
- Temporary MBS items 695 and 19000 for health assessments targeting women experiencing menopause or perimenopause
- Removal of MBS items for COVID-19 vaccine suitability assessments
For more information and future updates, visit the MBS Online News webpage.
Quarter 4 payment requirements for the General Practice in Aged Care Incentive
Patients participating in the General Practice in Aged Care Incentive (GPACI) since September 2024 may now be in quarter 4 (Q4) of their care period. To be eligible for Q4 incentive payments, both quarterly and annual servicing requirements must be met.
Patients who had the incentive added to their MyMedicare profile in the July-September 2024 quarter are now in Q4 of their 12-month care period.
To receive incentive payments for patients in Q4, both the practice and the responsible provider must deliver the quarterly servicing requirements AND the annual servicing requirements.
Each quarter:
- The practice and provider must deliver at least two regular services to the patient, each in a separate calendar month.
- The responsible provider must deliver at least one of the regular services. The other regular service can be delivered by either the responsible provider or an alternate provider.
In each 12-month annual care period:
- Two care planning services must be delivered by the responsible provider.
- Eight regular services must be delivered by an eligible provider linked to the same practice as the patient receiving the services.
Practices can utilise the eligibility forecast in HPOS to keep track of how they are progressing towards the requirements of the incentive.
If the responsible provider does not deliver the two care planning services by the end of the 12-month care period:
- The practice and the responsible provider will not receive the Q4 payment.
- The responsible provider must deliver at least one care planning service in Q1 of the following 12-month care period.
If the requirements are not met, the practice and provider will be ineligible for the incentive payments for that patient for the remainder of the patient’s new 12-month care period.
HPOS will notify practices and responsible providers if requirements are not met.
For further information, refer to the GPACI program guidelines.
For more information or support on GPACI, contact the Practice Assist Help Desk on 1800 2 ASSIST (1800 2 277 478) or 08 6278 7900 or via email practiceassist@wapha.org.au
MyMedicare accreditation exemption for non-traditional practices extended to 31 December 2026
The MyMedicare accreditation exemption for non-traditional practices choosing to participate in MyMedicare has been extended from 30 June 2025 until 31 December 2026.

The accreditation exemption is available to non-accredited practices (including sole providers) who deliver general practice services entirely through mobile and outreach models
- in rural settings
- in residential aged care
- in disability residential settings
- to First Nations Australians
- to people experiencing homelessness.
The extension is in recognition of the new definition of general practice for the purpose of accreditation, which may allow some non-accredited non-traditional practices to now become accredited. This extension aims to support non-accredited practices in considering their accreditation options under the National General Practice Accreditation Scheme. Practices currently utilising this MyMedicare exemption will not need to take any action to update the new end date.
After the end of the exemption period, all non-traditional practices will be subject to usual MyMedicare accreditation requirements, which includes a 12-month period to work towards accreditation.
Non-accredited practices who do not deliver general practice services entirely through mobile and outreach models, i.e., traditional practices, are not eligible for this exemption. Therefore, they are not affected by the 31 December 2026 date.
The MyMedicare accreditation requirements for traditional practices remain unchanged. That is non-accredited traditional practices continue to have 12 months to gain accreditation through a registered accreditation agency from the date they register in MyMedicare as a practice.
For more information or support on MyMedicare accreditation, contact the Practice Assist Help Desk on 1800 2 ASSIST (1800 2 277 478) or 08 6278 7900 or via email practiceassist@wapha.org.au

Become an RACGP accredited GP training provider – EOIs open
The RACGP is looking to increase GP training capacity for 2026 and beyond. As an RACGP accredited training site, your practice will have the opportunity to contribute to your community’s GP workforce needs and play a key role in shaping future GP registrars in your area.
You’ll also have access to RACGP support and resources, as well as financial incentives in the form of supervisor and teaching payments to assist with the training of GP registrars.
The RACGP is seeking expressions of interest from practices and supervisors in identified areas of need, who are passionate about teaching and meet the following requirements:
- RACGP Standards for general practice training
- Guide to training site and supervisor accreditation
- Codes and principles for training sites and supervisors
- National General Practice Accreditation (NGPA) Scheme accredited general practice status.
Any MM2-7 practice, or those in selected MM1 regions, can submit an EOI but those not identified as a priority and/or that do not meet the current need will be waitlisted and contacted as needed.
View the list of WA GP catchments and submit your EOI here.
Practices are encouraged to submit EOI applications a soon as possible to ensure you’re ready to receive registrars for the start of the RACGP 2026, 1 Semester.
Chronic Wound Consumables Scheme
The Chronic Wound Consumables Scheme (CWCS) will help eligible patients manage their chronic wounds. It will cover the full cost of products they need to heal, such as bandages, dressings and adhesives.

Health professionals will be eligible if they are:
- Aboriginal and Torres Strait Islander health practitioners
- medical practitioners in a primary care setting, including general practitioners
- registered nurses and nurse practitioners
- podiatrists.
Eligible health professionals will need to complete specified training to use the online portal.
For further information and contact details, visit the Department of Health, Disability and Ageing Chronic Wound Consumables Scheme page.
Revised antibiotic guidelines: New dosing calculators

The most extensive update to the Antibiotic guidelines includes three new dosing calculators.
The aminoglycosides amikacin, gentamicin and tobramycin are recommended for many infections in the guidelines because they continue to play an important role in the management of gram-negative infections. Aminoglycoside toxicity has led some clinicians to argue that less toxic antibiotics (e.g. carbapenems, broad-spectrum cephalosporins) should be used instead. The group developed initial dosing calculators for amikacin, gentamicin and tobramycin to ensure that when aminoglycosides are recommended, they are dosed correctly.
Hear one of our experts discuss the calculator development and how they should be used on our YouTube channel.
DVA prior pharmaceutical approval requests now available through HPOS
The Repatriation Pharmaceutical Benefits Scheme (RPBS) gives eligible Veteran Card holders access to a range of medicines and wound-care products, in addition to those available under the Pharmaceutical Benefits Scheme.
GPs or other health professionals can contact DVA to get approval for medicines under the RPBS. They may also seek prior approval to prescribe clinically appropriate medicines that are not included on the RPBS.

Options to contact the DVA Pharmacy team are listed below, including a new online channel:
- Online:
Health Professionals Online Service (HPOS) Secure Form Upload Portal
- Telephone:
Veterans’ Affairs Pharmaceutical Advisory 24/7 contact centre on 1800 552 580 - Post:
VAPAC – Department of Veterans’ Affairs
GPO Box 9998
BRISBANE QLD 4001
More information available here.
Evidence-based, patient-approved resources supporting safe opioid use
The Routine Opioid Outcome Monitoring (ROOM) Tool is a quick, validated resource to support regular review of opioid use. Patients can complete it themselves on paper or online in under five minutes, and it helps assess pain, function, dependence risk, mood and other key outcomes.
It’s part of a new Opioid Safety Toolkit funded by the Australian Government. Within the toolkit, patients can also build a personalised safety plan to understand their risks, overdose signs, and how to respond using naloxone, a free, easy-to-use, medicine recommended for everyone on long-term opioids.
The toolkit is a collaboration between Monash University, the Burnet Institute, the Pharmaceutical Society of Australia and Pain Australia.
Contact Prof. Nielsen at opioid.safety@monash.edu or visit //saferopioiduse.com.au/ for more information.
ScriptCheckWA registration now mandatory
As of 12 June, registration with ScriptCheckWA is now compulsory for all prescribers who prescribe monitored medicines for patients in Western Australia.
Registering is a simple four step process that will take about 10 minutes to complete. You will require your AHPRA number, date of birth and a unique email address only accessible to you.
Register here.
Use of ScriptCheckWA is strongly encouraged and provides prescribers with real-time information about current use including overuse.
More information is available at:
WA Virtual Emergency Department now available through healthdirect
In a new partnership with healthdirect Australia, eligible adults calling the healthdirect helpline on 1800 022 222, may be offered a WA Virtual Emergency Department (WAVED) consultation instead of being advised to self-present to a hospital emergency department.
If a patient’s emergency is deemed suitable to be assessed and treated at home, healthdirect will connect that patient to a senior emergency doctor via telehealth. The WAVED service is available 8am – 10pm, seven days per week for patients with low urgency conditions who are:
- 16 years and over
- Located in the Perth Metropolitan or Greater Bunbury areas
Free Heart Health Checks at the GP funded for another three years
The Australian Government has announced free Heart Health Checks provided by a GP will continue to be funded under Medicare Benefits Schedule (MBS item 699) for Australians aged 30 years and older.
The comprehensive cardiovascular disease risk assessment and ongoing management tool takes less than 30 minutes and aims to support GPs to identify the risk of heart attack or stroke in those patients who haven’t previously been diagnosed with heart disease.
Visit the Heart Foundation website for more information.
Abortion Legislation Reform: Information for GPs
It has been 12 months since the new abortion legislation was implemented. The amended laws have:
- Enabled GPs, nurse practitioners and endorsed midwives to prescribe the medical abortion medicine (MS-2 Step) within their scope of practice and training
- Removed the mandatory counselling requirement
- Increased the gestational limit at which an abortion may be performed
- Specified mandated obligations for all medical practitioners, even those who conscientiously object
New resources are now available:
For clinical queries regarding abortion care, you can call the free WA Health funded helpline 1800 4 Choice (1800 424 642) for advice.
Patients can also call 1800 4 Choice for information about pregnancy choices and abortion care options across Western Australia.
Measles alert for Metropolitan Perth
The WA Communicable Disease Control Directorate has issued a measles alert for Metropolitan Perth following a confirmed case in a recently returned overseas traveller.
General practice should be alert for measles, particularly among returned overseas travellers and ensure all practice staff have a high index of suspicion for measles in patients presenting with a febrile rash.
Read the Metropolitan Perth measles alert for more information including list of exposure sites and current recommendations for health professionals.
Notify suspected cases immediately to your local Public Health Unit by telephone (8am to 5pm Mon-Fri excluding public holidays) or to the Department of Health (after hours).

The importance of data-driven quality improvement activities

Data-driven quality improvement (QI) activities are essential for maintaining a high-performing practice. Delivering care that focuses on the needs of your region and specific patient demographics can assist with providing focused, patient-centred care and provide the following benefits:
- Better health outcomes.
- Improved patient and staff safety.
- More efficient use of resources, systems and workflows.
- Increased business sustainability.
- Enhanced practice-team culture.
To initiate meaningful QI activities, consider the steps below:
- Identify areas needing improvement.
- Assess practice data to understand the needs of the patient cohort and services.
- Utilise data tools offered by WA Primary Health Alliance (WAPHA) such as Primary Sense and the Primary Care Reporting Portal.
- Keep practice data up to date by archiving records of inactive patients.
- Get assistance from WAPHA’s Practice QI Coaches to help extract necessary information from data tools and your practice management software.
QI activities work best with a whole-of-practice-team approach to ensure that the people involved in delivering care are invested in the activity. This can lead to the following benefits:
- Improved patient outcomes.
- Empowered and engaged teams.
- Enhanced workplace satisfaction.
QI is nothing new, practices are doing it every day, probably without realising it. It is important to document QI activities so systems and processes can be reviewed to ensure continuing improvement in service delivery and patient outcomes. Key things to remember:
- Use templates for documentation from the Practice Assist QI Tool Kit webpage.
- Document activities so systems and processes can be regularly reviewed.
- Evaluate outcomes to see whether changes are leading to improvement.
- Learn from the outcomes to guide future activities and celebrate successes.
For further information or individualised support with QI, email WAPHA’s QI team via qi@wapha.org.au or call the Practice Assist help desk on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or email practiceassist@wapha.org.au
Primary Sense June release
Primary Sense is introducing new reports to help you manage patients.
This report includes important health data, such as pathology results, medication lists, and diagnoses, and allows you to easily filter and sort the information.
Key Features:
- Patient Criteria: Includes patients aged 18 and over who are actively attending the practice, excluding nursing home patients and those with palliative care codes.
- Pathology Results: Uses eGFR and ACR to monitor kidney function. Latest SBP is available from the diabetes report, and vaccination dates are included from the winter wellness report.
- Medications: Lists medications with recent activity and includes SLG2 inhibitors.
- Diagnosis and Conditions: Provides information on hypertension, smoking, diabetes, and BMI.
- Complexity Levels: Categorizes patients based on their health risks.
- Recommendations: Offers specific recommendations for patient reviews, medication assessments, and referrals.

This report identifies patients aged 50–70 who may be eligible for a funded low-dose CT (LDCT) scan. It includes smoking history, clinical indicators, and scan history, and is designed to be actionable and exportable for patient recall.
Practices can use this report to:
- Identify and recall eligible patients for screening, improving early detection and outcomes.
- Streamline workflows by exporting filtered patient lists directly into recall systems.
- Support clinical decision-making with detailed patient data, including smoking intensity and cessation history.
- Reduce administrative burden through automated report saving, export options, and persistent filters.
- Enhance patient safety and compliance by ensuring only appropriate patients are included and tracked.
For more information about Primary Sense, visit the Practice Assist Primary Sense webpage, call the Practice Assist help desk on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or email practiceassist@wapha.org.au
Access your practice data reports through the Primary Care Reporting Portal (PCRP)
General practices that share data with WA Primary Health Alliance for PIP QI can access their practice data reports through the Primary Care Reporting Portal (PCRP).
- My Practice Data Report – A comprehensive summary report for practices sharing data with WAPHA for PIP QI and quality improvement activities.
- News Feed – Stay updated with the latest news, issues, and information on the Primary Sense tool, along with other relevant details for general practice.
- Resources – Access manuals and guides to assist with using the portal and interpreting reports.
If your general practice shares data with WAPHA via Primary Sense and you have not received an email inviting your practice’s nominated administrator to access the PCRP, please contact the Practice Assist Help Desk on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or via email practiceassist@wapha.org.au
Are lost prescriptions impacting your practice?
Electronic prescriptions (e-scripts) are a key enabler of virtual healthcare and telehealth services but also offer benefits when providing health care face-to-face. E-scripts can reduce the workload for GPs and admin teams associated with reissuing lost paper scripts, enabling prescribers to modify, cancel and re-issue prescriptions instantly.
Did you know that patients can still get their e-scripts dispensed even if they have misplaced or accidentally deleted the token? All they need to do is register for an Active Script List (ASL).
An ASL is a consolidated list of all of the patient’s active electronic prescriptions (e-scripts) including repeats. After registering for ASL at a pharmacy patients can authorise any pharmacy to access and dispense their e-scripts from their ASL without needing to display the QR token.
ASL makes medication management easier for patients:
- taking multiple medications regularly
- that lose or struggle to keep track of their paper or electronic prescriptions
- without smartphones
- with chronic conditions or who rely on carers or support persons to assist with medication collection
Conformant apps like the my health app support patient-centred care by enabling patients to view and manage the active prescriptions in their ASL.
See this short video by the Australian Digital Health Agency for an example of ASL in action.
For more information or support on setting up and using e-scripts in your practice, contact the Practice Assist Help Desk on 1800 2 ASSIST (1800 2 277 478) or 08 6278 7900 or via email practiceassist@wapha.org.au

A message from the Australian Government Department of Health, Disability and Ageing on the flu vaccination
Annual vaccination is critical in preventing influenza (flu) and its complications. With flu season underway, yearly flu vaccination is recommended for all people aged 6 months and over.
The National Immunisation Program provides free flu vaccines to people at higher risk of complications, including:
- children aged 6 months to less than 5 years
- pregnant women at any stage of pregnancy
- people aged 65 years and over
- Aboriginal and Torres Strait Islander people aged 6 months and older
- people with certain medical conditions
The WA Department of Health also has a state-funded program which provides flu vaccines for:
- children aged 5 years to under 12 years
- persons experiencing homelessness or congregate living, 12 years to under 65 years
- until 30 June – any person 12 years to under 64 years
Health professionals can review the ATAGI statement on the administration of seasonal influenza vaccines. More influenza vaccination program advice is available here.
Correct administration of RSV vaccine and antibody products
The Therapeutic Goods Association (TGA) has recently released a Medicines Safety Update containing advice on how to avoid errors when administering RSV immunisations.
In response to reports about an increasing number of administration errors relating to RSV prevention Products, the TGA are reminding prescribers and vaccination provides that each product is specifically indicated for different patient groups. No adverse event was reported for most of the product administration error reports received by the TGA to date, but an administration error may lead to various problems, including unknown levels of protection for vaccine recipients.
The new immunisation products:
- Arexvy – is a vaccine used to prevent lower respiratory tract disease in individuals aged 60 years and older, or those aged 50–59 years who are at increased risk of RSV disease.
Arexvy was approved by the TGA on 14 January 2024.
- Abrysvo –is a vaccine given to pregnant women to prevent lower respiratory tract disease caused by RSV in their infants from birth through to 6 months of age.
It is also approved for use in individuals aged 60 years and older.
As of 3 February 2025, Abrysvo has been funded for pregnant women between 28 and 36 weeks’ gestation under the NIP.
- Beyfortus – (nirsevimab) is a human immunoglobulin monoclonal antibody given to infants and children to prevent RSV lower respiratory tract disease.
Beyfortus (nirsevimab) is delivered through state and territory immunisation programs.
Health professionals should note the indications for the different products and the circumstances of the administration errors outlined above.
Personnel at vaccination sites should undertake careful planning to prevent errors in prescribing, dispensing and administering RSV prevention products.
- Attend or watch any education and training on the differences in RSV immunisation products
- Us both generic and brand name when prescribing
- Improve storage practices – such as storing on different shelves in the vaccine fridge
- Follow recommended administration practices
If an error does occur report the administration error to SafeVac reporting via a WA Vaccine Safety Surveillance (WAVSS).
Clinical guidance on RSV immunisation product administration errors, including advice regarding the need for repeat doses, is available at: National Centre for Immunisation Research and Surveillance.
All doses still need to be reported to the Australian Immunisation Register.
Read the full safety update here.
A new hub for Department maternal vaccination materials

To equip pregnant women with information about vaccines that are recommended during pregnancy, the Australian Government Department of Health, Disability and Ageing has launched a dedicated mini-site on maternal vaccinations. The site includes information about RSV, whooping cough, and influenza maternal vaccinations and features a resource collection that includes a poster, brochure, and factsheets.
There are also dedicated resources for pregnant Aboriginal and Torres Strait Islander women, and translated resources available in Arabic, Mandarin, Cantonese, and Vietnamese.
Visit the site here.
Upcoming vaccine brand changes
The Department of Health, Disability, and Aging wishes to advise of an upcoming change to supply arrangements to states and territories under the National Immunisation Program (NIP) to take place from 1 July 2025.
From 1 July 2025, the supply of measles containing vaccines will move from two suppliers (GSK and CSL) to one (only GSK).
WA Health will continue to distribute doses of M-M-R® II (CSL) and Varivax (Varicella) (CSL) until they are exhausted. Once exhausted, orders will be supplied exclusively with GSK’s Priorix (MMR), Priorix-Tetra (MMRV), and Varilrix (Varicella).
Note: Due to shelf life, Priorix may be supplied before M-M-R® II.
Providers should continue to use their current stock of M-M-R® II and Varivax until it either expires or runs out.
There is no change to the vaccination schedule or the ordering process.
We encourage health professionals and stakeholders to subscribe to the NIP and NCVP email list to receive the latest NIP updates.
A refresh of immunisation resources on the NCIRS website
The National Centre for Immunisation Research and Surveillance (NCIRS) website features a range of resources to support all immunisation providers, including Sharing Knowledge about Immunisation (SKAI) tools to assist with immunisation conversations, information sheets, FAQs, decision aids, and safety data.
To read and download resources available, click here.

Adolescent and maternal vaccinations, plus a mid-winter illness report card
Presented by RACGP
3 July 2025 (7pm to 8pm AWST) webinar
Join infectious disease expert Prof. Paul Effler for a webinar concerning adolescent and maternal vaccinations, plus a WA mid-winter illness update. You’ll have the opportunity to ask questions during the Q&A. If you have a question prior, you can submit it upon registration.
Prof Paul Effler is the Senior Medical Advisor, Communicable Disease Control Directorate, Department of Health, Western Australia. Hosted by GP Dr Ramya Raman.
This webinar is delivered in partnership with the Department of Health Western Australia.
2025 RSV webinar
Presented by Immunisation Coalition
9 July 2025 (4pm to 5pm AWST) webinar
This webinar, hosted by the Immunisation Coalition will provide an overview of RSV epidemiology, disease burden and an update on the new NIP listed maternal RSV vaccine and monoclonal antibody State funded programs from an indication and usage perspective.
Consideration is also given to the TGA approved, yet currently unfunded vaccine for older adults, as tagged Recommended and Considered in the Australian Immunisation Handbook.
This information will be of interest to healthcare professionals providing care to pregnant women, young children, and the older adult population in preparation for possible future funded programs.
In particular, the webinar will be of interest to those healthcare professionals who are involved in the delivery of immunisation services.
Please note: There is a nominal fee of $14.95 for this webinar. All proceeds will support the development of the new Immunisation Coalition website, which aims to provide additional vaccination resources for healthcare professionals, especially primary care immunisers. The website is scheduled to launch in September.
Australian Vaccinology Course – boost your impact in immunisation
Presented by NCIRS in Partnership with The University of Sydney
28 August until 30 August 2025 (in-person)
The National Centre for Immunisation Research and Surveillance (NCIRS) has launched the inaugural Australian Vaccinology Course, a new in-person program designed for professionals seeking a deep, evidence-based understanding of vaccines, immunology and vaccination programs.
Informed and delivered by Australian and international experts, the immersive program will equip you with the critical knowledge and skills required to:
- confidently navigate the complex landscape of vaccine science and policymaking
- address immunisation program-related questions from diverse stakeholders play a pivotal role in improving vaccine uptake.
Whether you’re involved in policymaking, clinical practice, public health or research, this course will empower you to contribute meaningfully to local and national immunisation strategies; enhance vaccine decision-making processes; and become a trusted advocate for immunisation in your community and country.
The event will be held at the Q Station in Manly, Sydney from 28-30 August 2025, with a one-day option available to attend the Essential immunisation provider update on Saturday 30 August 2025.

National Lung Cancer Screening Program launches 1 July 2025
The National Lung Cancer Screening Program aims to achieve better health outcomes for Australians by detecting lung cancer early and saving lives. Early detection can lead to more effective treatment options and improved outcomes for patients.
The program screens for lung cancer in high-risk individuals using low-dose computed tomography (low-dose CT) scans. The program targets people with no signs or symptoms suggesting they may have lung cancer and:
- Are aged between 50 to 70 years old
- Who smoke tobacco cigarettes or have a history of cigarette smoking (quit within the last 10 years).
Your practice will play a critical role in supporting participation in the program.
Here are a few steps you can take to get your practice ready:
- Register and integrate your clinical software with the National Cancer Screening Register.
- Review and update smoking histories in your clinical records to identify patients who could be eligible.
To assist practices in identifying eligible cohorts for the program, Primary Sense has created a National Lung Cancer Screening Report with their latest update.
This report assists practices in proactively identifying patients eligible for the low-dose computed tomography (LDCT) scan, as per the eligibility criteria. It will also support GPs in their vital role in the program, as they assess eligibility and refer eligible individuals for an LDCT scan.>
See the Primary Sense Desktop Lung Cancer Screening guide for more information and guidance.
Clinician Assist is currently working on a Lung Cancer Screening Pathway which will feature all the relevant pathway information and resources needed to be involved in the screening program.
To register and access Clinician Assist, click here.
- Resources for health professionals and consumers are available on the Department of Health, Disability and Ageing website.
- Complete the accredited eLearning modules for the program available through the Lung Foundation Australia Lung Learning Hub.
- Sign up and listen to the National Lung Cancer Screening Program Health Workforce Education Webinar on how to prepare for and integrate the program in your practice.
For more information, click here.

Public consultation to include COVID-19 vaccine in Immunisation Handbook
The Australian Technical Advisory Group on Immunisations (ATAGI) recommendations for the use of COVID-19 vaccines were first published in the Australian Immunisation Handbook in 2023.
ATAGI has revised its advice many times because the disease and the vaccines were changing quickly.
Now that things have become more stable and will not change as often, ATAGI is asking for public input on the recommendations.
This public consultation document can be accessed on Citizen Space here.
To make a submission, please click on the “Online Survey” link where you will be directed to some targeted questions. The public consultation will close on 11 July 2025.
If you have any inquiries regarding this consultation, please do not hesitate to contact the ATAGI secretariat via email.
Help shape the accreditation of medical imaging providers
The Australian Commission on Safety and Quality in Health Care is undertaking a consultation on the Australian Safety and Quality Medical Imaging Accreditation Scheme. Medical Imaging providers will be assessed against the National Safety and Quality Medical Imaging Standards under the ASQMIA Scheme. This scheme will replace the Diagnostic Imaging Accreditation Scheme.
The current desktop assessment does not test the effectiveness of day-to-day safety or quality systems. The introduction of onsite, virtual and short notice assessment will be a more rigorous review of the processes of clinical practice.
The Commission wants to ensure the proposed Australian Safety and Quality Medical Imaging Accreditation Scheme meets the sectors’ and consumers’ expectations regarding safety and quality in medical imaging.
You are invited to share your experiences, review the proposed accreditation scheme, and offer your insights on safety and quality in medical imaging. Complete the survey by Friday 18 July.

Go Dry This July

Dry July is a fundraiser that encourages you to go alcohol-free in July to raise funds for people affected by cancer.
The funds raised during Dry July will provide invaluable services for cancer patients, their families and carers – whether it’s a lift to a life-saving appointment, guidance from a specialist nurse, connection to an informative voice, access to therapy programs or a bed close to treatment.
Having a month off alcohol also has great health benefits, such as sleeping better, having more energy and of course, no hangovers! So you’re not only helping others, but you’re also helping yourself. It’s a win-win!
Learn more about Go Dry This July or view the Dry July Workplaces Hub for more information on how to participate.
World Endometriosis Congress: WA pelvic pain clinic presents unique model of care
With endometriosis affecting one in nine Australian women, the Australian Government has funded 22 endometriosis and pelvic pain clinics across Australia to build the capacity of primary care to manage this condition and improve access to expert, multidisciplinary services. This number is expected to grow to a total of 33 clinics nationally over the next three years.
Last month, a small team from The Garden Pelvic Pain Clinic in Murdoch presented their model of care at the World Endometriosis Congress in Sydney. Their presentation highlighted the importance of a multidisciplinary approach to supporting patients, emphasising collaboration to deliver holistic and compassionate care. Initially funded to support people with endometriosis and chronic pelvic pain, the clinic has broadened its scope to deliver comprehensive care for patients.
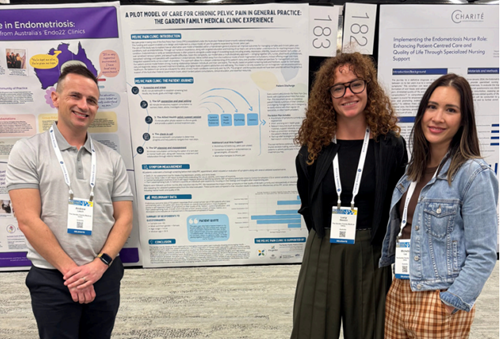
The presentation from Dr Andrew Leech, Dr Michelle Guy and Miss Lucy Stewart attracted significant interest from participants, who were eager to learn about nurse-led clinics, telehealth models, and services aimed at populations with limited access to specialised care.
Read their recap from the World Endometriosis Congress May 2025.
The Garden Family Medical Centre is part of the Australian Government’s Endometriosis and Pelvic Pain Clinic initiative supported by WA Primary Health Alliance under the Primary Health Networks Program.

STI and BBV Refresher Series
Presented by WA Primary Health Alliance
26 June and 24 July 2025 (6pm to 6:15pm)
Join us for a series of training webinars designed to enhance your knowledge and skills on syphilis in general practice, including interpreting results, initiating treatment, contact tracing, co-infections and hepatitis C.
Webinar 1: Incorporating STI testing into everyday care
The first webinar of the series on Thursday 26 June will explore sexual health assessments in general practice and cover the following topics:
- Normalising STI testing in everyday consults.
- Groups to target for opt-out screening.
- Taking a sexual health history.
- Tests to offer.
Webinar 2: Interpreting STI results and initiating treatment
The second webinar on Thursday 24 July will explore sexual health assessments in general practice and how to interpret syphilis serology and initiate treatment.
Webinar Series: Dementia Demystified
Immediate Post Diagnostic Management – Webinar 3
3 July 2025 (6pm to 7pm)

Join us for the third webinar in the Dementia Demystified series by Dementia Training Australia’s expert medical education team.
This webinar will cover the following topics:
- Recognise the changing goals of care with the progression of dementia.
- Implement an effective management plan for people living with dementia.
The webinar is accredited for 1 RACGP EA CPD hour.
To find out more, view the flyer and register webinar 3 today.
Webinar: Adolescent and maternal vaccinations, plus a mid-winter illness season report card
RACGP and WA Health
3 July 2025 (7pm to 8pm)
Infectious disease expert Professor Paul Effler will present WA data on coverage and safety for adolescent and maternal immunisations, including the newly registered Abrysvo RSV vaccine. He will also provide a ‘mid-winter report card’ on how WA is tracking with respect to important respiratory pathogens including influenza, RSV and COVID-19.
Find out more and register.
WA HIV Prescriber Update – ARV Update
Presented by ASHM
15 July 2025 (7pm to 8pm)

Stay up to date with the latest in HIV treatment and prevention, including LEN and CAB/RPV, and explore key updates to the ARV guidelines.
This session will cover ASHM resources, the LAI HIV Treatment Tool, and best practices for transitioning patients from oral regimens to injectables, with a focus on patient-centered care.
To find out more and register, view the flyer.
WA Hepatitis B for Nurses and Midwives
Presented by ASHM
25 July 2025 (10am to 3pm)
This course will provide nursing and midwifery professionals with advanced practical skills and knowledge in hepatitis B nursing.
The face-to-face course will introduce the epidemiology of hepatitis B, vaccination and prevention, understanding testing and serology, initial assessment and the cultural context of hepatitis B nursing and midwifery. The second half of the day will involve case discussions and presentations on monitoring and management of chronic hepatitis B and HCC surveillance.
To find out more and register, view the flyer.
WA Ear and Hearing Health Forum 2025
Presented by Rural Health West on behalf of the Aboriginal Health Council of WA and the WA Child Ear Health Strategy
7 August and 8 August 2025

Rural Health West on behalf of its partners the Aboriginal Health Council of WA and the WA Child Ear Health Strategy invite health professionals to attend the WA Ear and Hearing Health Forum 2025.
The two-day forum will focus on regional ear health initiatives, successes and challenges, technologies and research in ear and hearing health through interactive discussions and upskilling sessions.
The forum has been developed to provide medical and primary health care professionals an opportunity to connect with peers, hear from researchers who are innovating the space and learn about current ear health initiatives being implemented across the nation and state.
To find out more and register, visit the forum webpage.
Register now for the Aboriginal Health Conference 2025
Delivered by Rural Health West in partnership with WA Country Health Service
9 August and 10 August 2025

The Aboriginal Health Conference 2025 will provide an opportunity to come together and learn from each other. Through presentations, panel sessions, case study discussions and workshops, we will deliver an engaging and informative conference program for delegates.
The 2025 theme Writing the Narrative – Telling Our Stories highlights the power of stories and how they shape identities, preserve culture and influence change.
The conference program features five streams, providing comprehensive insights into crucial aspects of Aboriginal health:
- Building trust and collaborating with community
- Chronic disease: Prevention, management, and community-led solutions
- Healing and wellbeing through storytelling
- Sexual health: Empowering communities with knowledge and access
- Supporting wellbeing from birth to eldership
To find out more, view.
Early career GP conference
Delivered by RACGP
9 August and 10 August 2025 (10am to 3pm

Explore the things you need to know as an early career GP; preparing you for what’s ahead.
Designed by GPs for GPs, the weekend offers relevant topics for New Fellows, GPs in Training and IMGs. This year’s theme is “Building our futures” and includes talks on finance, career sustainability, conquering CPD and technology in general practice.
Sessions confirmed so far:
- Q&A with RACGP President and Vice President – Dr Michael Wright and Dr Ramya Raman
- Personal finance fact and fiction – Dr Jonathan Tan
- Ways to make technology work for you – Dr Sean Stevens
- Tailoring your practice to suit the needs of you and your patients – Dr Andrew Leech
- Ten things I wish I’d known as a New Fellow – Dr Sean Stevens and Dr Tim Koh (Live The Good GP podcast recording)
- Managing uncertainty and developing grit as a rural general practitioner – Dr Michael Clements
- Sole Trader 101 – Rosa Murray
- The secret life of a Practice Manager – Natalie Watts, Lockridge Medical Centre
- Grassroots patient advocacy and education – Dr Andrew Leech
- Conquering CPD – Hatha McDivitt, RACGP WA CPD Coordinator
- New Fellows committee discussion panel
… and more to come!
All New Fellows and GPs on a training pathway towards Fellowship are encouraged to attend.
Forward this event to a colleague who may find this conference useful.
Nurse Forum: Celebrating and Advancing Primary Care
Presented by WA Primary Health Alliance
13 August (6pm – 8pm)
Join us for an in-person evening event recognising and supporting practice nurses working in general practice across the Perth metropolitan region. The forum will offer valuable networking opportunities and deliver tailored professional support for general practice nurses, fostering peer connection, shared learning and practical tools to enhance their role in primary care.
Find out more and register.
Register now for a Clinician Assist WA live demonstration
Presented by Clinician Assist WA
Multiple Times & Dates Online

Clinician Assist WA is a secure website providing GPs and other health professionals with guidance for assessing, managing and referring patients across Western Australia. It has replaced HealthPathways WA, offering the same trusted local guidance, features and functionality and remains available at no cost.
The Clinician Assist WA team will run online demonstrations facilitated by a GP Clinical Editor throughout 2025 to support users. These sessions will demonstrate how to maximise integration of Clinician Assist WA into your clinical practice. Learn key functionalities of the website and how to access condition specific tools and resources, Referral Access Criteria (RAC) (where available), GPbook Specialist Directory and visiting specialist rosters.
Sessions have been approved for 1 CPD Educational Hour with RACGP and will be held online on the following dates:
Demonstrations are open to general practitioners, general practice staff and other health professionals registered to practice in WA.
National Kidney Summit 2025
Presented by Kidney Health Australia
10 October 2025 (full-day event)
Kidney Health Australia is bringing together national stakeholders to inform a National Kidney Summit with the theme ‘CKD in Crisis. Detect Early. Act Now. Save Lives.’
The Summit will:
- Challenge the current approach to CKD care.
- Identify vital levers and actions to drive the early detection, diagnosis and management of CKD.
- Develop urgent solutions to drive collaborative health care reform to improve outcomes for Australians living with CKD.
This full-day summit in Sydney will bring together thought leaders, health care professionals, researchers, consumers and advocates to explore opportunities and co-design impactful strategies.
Register your interest via the online form.
Other Webinars, Events & Workshops
| FPAA Certificate in Reproductive and Sexual Health for Doctors Presented by SHQ 30 June to 4 July |
| BreastScreen WA visit to Derby Presented by BreastScreen WA 4 July to 17 July |
| Culturally Responsive Care and Hepatitis B Presented by ASHM 10 July |
| Course in Wound Closure Presented by Benchmarque Group 11 July |
| BreastScreen WA visit to Southern Cross Presented by BreastScreen WA 11 July to 16 July |
| BreastScreen WA visit to Claremont Presented by BreastScreen WA 14 July to 01 August |
| BreastScreen WA visit to Yanchep Presented by BreastScreen WA 14 July to 22 August |
| WA HIV Prescriber Update – ARV Update Presented by ASHM 15 July |
| BreastScreen WA visit to Coolgardie Presented by BreastScreen WA 18 July to 21 July |
| BreastScreen WA visit to Fitzroy Crossing Presented by BreastScreen WA 21 July to 5 August |
| WA HIV Prescriber Update – HIV and the Heart & Mind Presented by ASHM 29 July |
| Wesley LifeForce Suicide Prevention Training Primary Care Support Staff Workshop (Rockingham) Presented by Wesley LifeForce 16 September |
| Wesley LifeForce Suicide Prevention Training Primary Care Support Staff Workshop (Mandurah) Presented by Wesley LifeForce 17 September |
| ACNP National Conference Presented by Australian College of Nurse Practitioners (ACNP) 29 October to 31 October |
| Asia Pacific Autism Conference (APAC) Presented by Autism Association of Western Australia 13 November to 15 November |
Acknowledgement
WA Primary Health Alliance acknowledges and pays respect to the Traditional Owners and Elders of this country and recognises the significant importance of their cultural heritage, values and beliefs and how these contribute to the positive health and wellbeing of the whole community.


