Issue 220 – 15 May 2025

| Welcome to Practice Connect, a fortnightly update for practice managers, principals, nurses and administration staff on relevant issues, upcoming events and education. |

MyMedicare updates and reminders

MyMedicare accreditation exemption date extended to 31 December 2026
The Department of Health and Aged Care is pleased to advise that the accreditation exemption for non-traditional practices choosing to participate in MyMedicare has been extended from 30 June 2025 until 31 December 2026.
The accreditation exemption is available to non-accredited practices (including sole providers) who deliver general practice services entirely through mobile and outreach models:
- in rural settings
- in residential aged care
- in disability residential settings
- to First Nations Australians
- to people experiencing homelessness.
The extension is in recognition of the new definition of general practice for the purpose of accreditation, which may allow some non-accredited practices to now become accredited. This extension aims to support non-accredited practices in considering their accreditation options under the National General Practice Accreditation Scheme.
Practices currently utilising this MyMedicare exemption will not need to take any action to update the new end date.
Reminders: turn on your HPOS mailbox notifications
We know you receive a lot of correspondence via your individual and/or organisation Health Professional Online Services (HPOS) mailboxes.
- While some of these may be statements or everyday notifications, some of these are important and require action.
- Turn on notifications to receive alerts for new messages, to save you having to check regularly for new mail.
- Now that the first MyMedicare Incentive is in place, please make sure you action any notifications as required, e.g. failed payments.
Payments (January – March 2025 quarter) and reassessments
Payments for the MyMedicare General Practice in Aged Care Incentive quarterly assessment for January – March 2025 have been processed and notifications have been sent via Health Professional Online Services (HPOS) mailboxes. The time taken to receive funds is dependent on individual financial institutions.
- Remember to check your HPOS notifications for any requiring action, e.g. failed payments due to missing or incorrect bank account details.
- IMPORTANT MESSAGE FOR RESPONSIBLE PROVIDERS: Add your (responsible provider) bank account details to HPOS specifically for the MyMedicare program, otherwise the GPACI payments won’t be able to be received. It is essential that this step is completed as it will ensure completion of GPACI registration.
- REASSESSMENTS: There has been a delay in reassessing previous quarterly payments and therefore a delay in adjustments, including additional payments that practices and providers may be expecting. When reassessments have been processed, you will be notified of any adjustments to previous payments via your HPOS mailbox.
GP Activation Series for Chronic Conditions Management – Activity 3

WA Primary Health Alliance is supporting early change management with general practices in advance of Chronic Conditions Management (CCM) MBS item changes scheduled to come into effect 1 July 2025. We invite your practice to participate in our CCM Activation Series to make small manageable changes to maximise the benefits of MyMedicare for your general practice and your patients.
Activity 3 – MyMedicare patient engagement and registration communications
Activity 3 takes a focus on enhancing MyMedicare patient engagement and registration communications. Outcomes of Activity 3 for your practice include:
- Understand how MyMedicare is evolving, and the current and future benefits.
- Develop a shared practice team perspective of how MyMedicare aligns with your practice’s approach to patient care.
- Develop key messages, benefits and talking points that your practice team can use to consistently communicate to patients about Chronic Conditions Management and MyMedicare.
- Develop a plan for targeting patient populations using different communication mediums and channels to increase MyMedicare registration for regular patients of your practice.
Click here to download your copy of the Activity 3 slide pack with activities for your practice and practice team.
You can find other activities previously released as part of the CCM Activation Series below:
- Activity 1 – The aim of this activity is to engage patients returning to your practice for Chronic Disease Management Plans and team care arrangements in MyMedicare, and regular reviews in the future.
- Activity 2 – The aim of this activity is to raise awareness among your practice team of MyMedicare and Chronic Conditions Management changes and support your team to explore and document their roles in both MyMedicare and Chronic Conditions Management.
Information on quality improvement for your practice, including Plan-Do-Study-Act templates. Can be found on our Practice Assist Quality Improvement Tool Kit page. If you would like support from our team to implement this activity, please contact our Quality Improvement Coaches by emailing qi@wapha.org.au
Catch the replay: Transform your practice with our Chronic Disease Management webinar
Did you miss our live webinar on chronic disease management? Watch the recording to gain valuable insights to enhance your practice.
Our recent webinar provided general practice staff with essential tools and strategies for effective chronic disease management. The session covered a range of critical topics, including:
- Understanding the fundamentals of chronic disease management: Learn the basics and build a strong foundation.
- Developing personalised care plans for patients: Tailor your approach to meet individual patient needs.
- Implementing evidence-based practices in daily clinical routines: Integrate proven methods into your everyday work.
- Utilising technology and data to enhance patient outcomes: Leverage modern tools to improve care.
- Collaborating with multidisciplinary teams for holistic care: Work seamlessly with other health care professionals to provide comprehensive care.
Featuring our expert Quality Improvement (QI) Coaches, the webinar included interactive discussions and practical case studies, ensuring that you can apply what you learn directly to your practice. Whether you’re new to chronic disease management or looking to refine your skills, this series offers valuable insights and actionable takeaways.
Don’t miss out on this opportunity to elevate your practice and improve patient care. Watch the recording now and take the first step towards better chronic disease management.
Stay tuned for more educational events and resources to support your professional growth.
Our Practice Assist Quality Improvement Tool Kit provides a comprehensive suite of resources and information to help practices on their QI journey.
Our dedicated team of QI Coaches are available to assist you in establishing and enhancing QI in your practice.
To connect with your local QI coach email QI@wapha.org.auḥ
New resources to support proposed bulk billing incentive measures

The Australian Government Department of Health and Aged Care (DoHAC) has developed a suite of new resources to support the proposed changes to bulk billing incentives in general practice.
Pending legislative approval, the Bulk Billing Practice Incentive Program, is due to come into effect from 1 November 2025. New resources relating to the Program include:
- Bulk Billing Practice Incentive Program: Eligible services
- Bulk Billing Practice Incentive Program: Frequently asked questions for practices and providers
- The impact of bulk billing investments on GP earnings and billings (discussion paper)
More information on the changes is available on the DoHAC website.
WA Primary Health Alliance will continue to share the latest updates on this proposed initiative as soon as they become available.
Improving early detection and management of chronic heart failure in the South West
Nannup Medical Centre in the South West region of Western Australia is participating in the second phase of the WA Primary Health Alliance funded Chronic Heart Failure (CHF) Pilot Project, which provides the practice with an on-site, non-dispensing pharmacist for 15 hours a week, over a 12-month period.
Betty White, Practice Manager at Nannup Medical Centre, explained that their dedicated team, led by the non-dispensing pharmacist, has forged an innovative partnership with Advara HeartCare to provide travelling cardiovascular services, including free echocardiograms, which are helping to improve the early detection and management of CHF among their patients.
“One of the major challenges historically faced by Nannup Medical Centre has been the limited access to essential diagnostic tools such as an echocardiogram for our patients. The burden on older patients to travel to larger facilities is a significant barrier that forces many patients to rely on brain natriuretic peptide (BNP) tests instead.
“Providing access to an echocardiogram is a vital step in the diagnosis process for CHF, which is improving the early detection and management of CHF among our patients, and ultimately helping to avoid hospitalisations,” Mrs White said.
For further information about assisting patients with CHF, call the Practice Assist help desk on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or email practiceassist@wapha.org.au
Quit centre resources for health professionals

Supported by funding from the Australian Government Department of Health and Aged Care, the Quit Centre is a national online resource developed by health professionals for health professionals.
At Quit Centre you will find clinical guidelines, online training and education and events to support you in delivering smoking and vaping cessation care in general practice.
Tailored resources and information for general practice are available here.
New WA service supporting hepatitis B management in primary care
To better support primary health care professionals to monitor, treat and manage patients diagnosed with chronic hepatitis B, GPs and practice nurses can now access direct clinical support, education and the latest advice on managing patients living with this viral infection.
Launched in January 2025 as a joint initiative between the WA Department of Health and Royal Perth Hospital (RPH), the statewide hepatitis B service is monitored Monday to Friday with a two-business day response time, with advice provided by either email, phone/video call or an in-person visit.
Access the service by emailing HepBHubWA@health.wa.gov.au
Free mobile liver scans (Fibroscan®) are also available via outreach clinics in metropolitan general practices/health services. Contact RPH hepatology nurse practitioner, Adam Gregson adam.gregson@health.wa.gov.au for further information.
ACCRM Rural Practice Community Support Grant Guidelines
The ACRRM Rural Community Support Grant provides remote, rural and regional communities in MMM 4-7 locations across Australia the opportunity to access funds for a broad range of health care related initiatives that directly and clearly benefit local communities.
Grants of up to $50,000 are available for a broad range of rural generalist community-led initiatives that directly and clearly benefit rural generalist training and recruitment of doctors to our rural and remote communities. Grants will be awarded to proposals that seek to link in ACRRM registrars to address improvement in the following categories:
- Education and training
- Recruitment and retention
- First Nations support
- University partnerships and training pathway development
ACRRM is seeking applications from training posts, rural generalists, health services or local communities’ groups that link to ACRRM registrars that strengthen GP training, recruitment and retention for smaller communities.
Read the Community Grants Fact Sheet and the 2025 Flexible funds FAQs for further information.

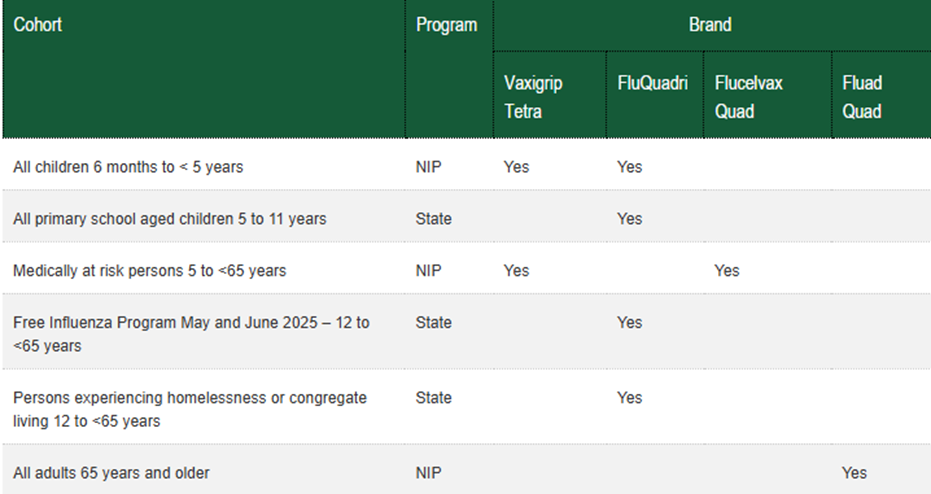
2025 influenza vaccination schedule
All Western Australians can access a free flu immunisation during the months of May and June this year, with some cohorts eligible for a free flu vaccine all season.
Immunisation is a safe and effective way to prevent from serious disease caused by influenza. All persons aged 6 months and over are encouraged to get the seasonal influenza vaccination.
The best time to get the influenza vaccine is before influenza season in late April or May. The influenza vaccine is available at any time during the influenza season, which is generally June to September.
After receiving the immunisation, it can take up to 2 weeks for the body to develop immunity and protect from influenza.
While the highest level of protection is in the first 3 to 4 months, encourage your patients that it is never too late to get vaccinated as influenza can be present in the community all year.
For more information visit WA Health’s webpage: Free influenza vaccine program May and June 2025.
Preparing for co-administration of COVID-19 and influenza vaccinations in 2025
WA rates of COVID-19 vaccinations have slowed in the last year, especially amongst people from at-risk communities.
COVID-19 vaccines can be co-administered with influenza (and other vaccines) in people aged five years or older to increase uptake and improve protection against both diseases.
Co-administering vaccines can offer logistical benefits, reduce costs, and potentially boost vaccine uptake.
The National Centre for Immunisation Research and Surveillance have developed Co-administration of vaccines for adults: a guide for immunisation providers .
Steps your practice can take now to prepare for the remainder of the winter season:
Step 1: Update your reminder message to increase awareness of co-administration service availability for influenza and COVID-19.
Step 2: Prepare your list of reminders to eligible patients (SMS, email, letter).
Step 3: Update your webpage information to reflect current COVID-19 and influenza vaccination advice, along with your clinic details.
Step 4 Update your online booking platform: Consider offering co-administration of COVID-19 and influenza vaccines where appropriate in a single appointment instead of two separate appointments.
Further information on COVID-19 vaccines and co-administration is available in the COVID-19 chapter of the Australian Immunisation Handbook.
Consider offering vaccines as a package this winter
At the recent WA Primary Health Alliance (WAPHA) Immunisation – Winter Wellness webinar (10 April 2025), presented by Professor Paul Effler and Professor Christopher Blyth, vaccine providers were encouraged to consider the co-administration of vaccines for influenza, COVID-19, pneumococcal and RSV.
Prof Effler is the Senior Medical Advisor at the WA Department of Health Communicable Disease Control Directorate and Prof Blyth is head of the Wesfarmers Centre of Vaccines and Infectious Diseases at the University of Western Australia and an Infectious Diseases Physician at Perth Children’s Hospital.
View the updated guide on co-administration of vaccines for adults from the National Centre for Immunisation Research and Surveillance here.
Watch the video of the Immunisation – Winter Wellness webinar here.
WAPHA’s role in COVID-19 management

WA Primary Health Alliance (WAPHA) has been involved in WA’s COVID-19 response, from the early days of the pandemic to the transition of COVID-19 into normal immunisation practice for respiratory illness.
In 2025, WAPHA continues to support existing local solutions to enable fair and timely access to vaccines. We are also working with the Australian Government Department of Health and Aged Care on a transition strategy for COVID-19.
For more information and resources, visit our webpages below:
To read further reflections on ‘WAPHA’s role in COVID-19 management’ click here.
Aboriginal Health Council of WA measles resources

The Aboriginal Health Council of WA (AHCWA) has developed several resources to support the WA Measles Immunisation Program. The resources can be found on their website and include:
Checklist for clinics – prepare for measles and a checklist for when responding to a suspected measles case in your clinic.
|
Measles prevention campaign – poster and social tiles
|
Measles response campaign – poster and social tiles
|
To access the posters and tiles, click here.
Refreshed immunocompromised chapter in the Australian Immunisation Handbook
A major expansion of the Australian Immunisation Handbook chapter on vaccination for people who are immunocompromised has been published, in a significant enhancement of guidelines relating to a complex area of immunisation practice.
While overall recommendations have remained unchanged, the refreshed chapter now includes more detailed advice on vaccination in people with a wide range of medical conditions and levels of immunocompromise.
It includes clear definitions of immunocompetence, immunosuppression and immunomodulation as well as levels of immunocompromise – which are categorised as mild, moderate or severe – along with several new tables that offer specific guidance relating to a wide range of immunocompromising conditions.
The chapter covers topics including inborn errors of immunity, secondary immunodeficiencies due to medical conditions or therapies, asplenia, exposure to immunosuppression in utero, immunocompromised close contacts and immunocompromised travellers.
People who are immunocompromised have an increased risk of severe illness or death from many vaccine preventable diseases, and their vaccination history – as well as potential contraindications to live vaccines – must be assessed carefully.
Access the Vaccination for people who are immunocompromised chapter.
AIR access for residential aged care homes
Facility and clinical managers can now apply on behalf of a residential aged care homes to become a recognised vaccination provider with the AIR.
This will support facility and clinical managers in organising vaccinations for residents living in care facilities by allowing them to access the AIR to identify residents who may be due or overdue for vaccines and to report vaccinations administered within the facility.
Information on the AIR can only be collected, used and disclosed for the purposes set out in the AIR Act, in line with the Australian Immunisation Register Rule 2015 (AIR Rule) and the Privacy Act. The AIR Act also contains protections and restrictions on how information in the AIR can be handled and who can use it.
Recognised immunisation providers can only use protected AIR information if it is for a permitted purpose. This includes (but is not limited to) the following:
- Checking an individual’s vaccination status
- Advising an individual when they are due to receive doses of a vaccine
- Certifying when a course of vaccination has been completed
This access does not authorise facilities to administer vaccines.
For further information, click here.
Immunisation Coalition – Annual Immunisation Forum
Presented by Immunisation Coalition
Friday 13 June 2025 (7.00am – 3.00pm AWST)
The 9th Annual Immunisation Forum (AIF) hybrid event will take a place at the Adelaide Convention Centre in Adelaide on 13 June 2025.
The meeting is ideal for GPs, practice nurses, specialists, pharmacists and other immunisation specialists.
The program covers the following topics: a look into aged care, new vaccines for the elderly, adjuvanted vaccines, vaccinations in primary care and pharmacy, managing vaccine hesitancy, targeting at-risk populations and addressing the vaccine gap of First Nations peoples.
This is a free CPD accredited (for online participation) meeting for a national audience.
Register for online attendance – via Zoom.

National Lung Cancer Screening Program resources now available

The National Lung Cancer Screening Program launches in July 2025.
General practice will play a critical role by increasing awareness of and supporting participation in the program.
Here are a few steps health care providers can take to get ready for July 2025:
- Find information and resources available on the Department of Health and Aged Care’s website including the Get your practice ready for the National Lung Cancer Screening Program resource to support practices prepare for the program and the Program Guidelines which support health care professionals and support workers to navigate through each step of the screening and assessment pathway.
- Register with the National Aboriginal Community Controlled Health Organisation to be notified when the Aboriginal and Torres Strait Islander resources for the program are available, and ensure practices have undertaken formal cultural safety training, which will assist health care providers in fostering and providing culturally safe care to Aboriginal and Torres Strait Islander peoples.
- Complete the CPD accredited eLearning modules for the program available through the Lung Foundation Australia Lung Learning Hub.
- The eLearning is accredited with Royal Australian College of General Practitioners, Australian Primary Health Care Nurses Association, National Association of Aboriginal and Torres Strait Islander Health Workers and Practitioners, and Australian College of Rural and Remote Medicine.
- On 15 April 2025 the Australian Government, National Aboriginal Community Controlled Health Organisation and Lung Foundation hosted a webinar focused on how to prepare for and integrate the program in your practice. Listen to the webinar recording here.
- Register and integrate with the National Cancer Screening Register for enrolment, monitoring and scan reporting.
- Review and update smoking history practice data in clinical records to identify patients who could be eligible.
For more information, visit www.health.gov.au/nlcsp
If you have any questions about the program and how you can become involved and support the program, email lungcancerscreening@health.gov.au
Bowel Cancer Awareness in June

This June, Cancer Council WA is encouraging all general practices to host a bowel health display, to help raise awareness about how patients can reduce their risk of bowel cancer.
To assist practices, they have collated a range of free resources focused on prevention, screening, and symptom awareness that practices can order and use to create their stall.
Practices that take part and send Cancer Council WA a photo of their display will go in the draw to win a prize.
For further information, click here.

Immunisation provider survey to help improve access to immunisation information in WA

WA Health is exploring better ways for providers and the public to access immunisation advice.
WA Health is seeking to understand more about your information needs when you have immunisation-related queries so they can provide a service that meets your needs.
All WA immunisation providers are asked to fill in the short survey in the link below.
The survey should take less than 5 minutes to complete.
Your responses will help WA Health improve access to immunisation information and support in Western Australia.
The survey will be open until 23 May 2025.

What’s your plan during National Palliative Care Week?
This year’s National Palliative Care Week (11-17 May), asks a simple, yet powerful question, “What’s your plan?” It’s a direct approach to Australians and their loved ones to talk about what matters most at the end of life and to make a plan that empowers and respects their choices during the last years, months, and days of life.
General practice is often the first point of contact for patients navigating serious illness and is ideally placed to initiate early palliative care discussions. Palliative care is not just about final days of life – it is about improving quality of life at any stage of a life-limiting condition.
What’s your plan prompts health professionals to become familiar with their patients’ values and end-of-life wishes through:
- engaging in conversations about end-of-life care
- prioritising advance care planning
- co-ordinating multidisciplinary care
- providing care that respects an individuals’ values and preferences
- referring early when specialist palliative care services are required.
Practices can help to raise awareness during National Palliative Care Week by downloading and sharing campaign resources through your practice channels and directing your audience to visit palliativecare.org.au
The Greater Choice for At Home Palliative Care measure
This Primary Health Network initiative being implemented by WA Primary Health Alliance (WAPHA) aims to improve access to quality palliative care at home. As a result, nine practices across WA have successfully integrated advance care planning into all routine 75+ and Aboriginal health assessments as well as embedding the same process into GP management plans for patients with complex chronic conditions.
Primary Sense Palliative Care Report
To assist with identifying patients who may benefit from a palliative approach Primary Sense has released the Palliative Care Report. This report highlights 1-2 per cent of patients who may be considered for palliative care discussions at the practice and/or discussions around implementing an advanced care plan.
Evidence-based clinical assessment tools
The Symptom Assessment Scale and Australia-modified Karnofsky Performance Scale can be being used to support symptom assessment and identify predicted deterioration/need for increased support services at home. These tools aim to reduce the risk of persistent/escalating symptoms and carer strain which may contribute to preventable hospital presentation. These tools also support identification of need to refer to specialist palliative care services.
Palliative care quality improvement opportunities
Some quality improvement (QI) opportunities around palliative care include:
- Create a process to ensure all clinical staff complete palliative care training
- Create a process to ensure all staff complete advance care planning training
- Download the Primary Sense – Palliative Care Report
- Identify and recall ATSI patients who may be considered for ACP and/or Palliative Care Planning. Consider prioritising patients with an ACG score 5
- Use the existing appointment tab to ‘flag’ patients for an ACP discussion who already have a scheduled appointment in the diary
- Create a process to ensure all clinical staff have created a Clinician Assist WA log-in and are familiar with the palliative care and advance care planning clinical pathways
WAPHA’s QI Coaches can support practices with completing PDSA cycles through providing guidance on running reports and interrogating data using various software and tools. Email QI@wapha.org.au to connect with your local WAPHA QI coach.
More palliative care resources for general practice
Visit the WAPHA website to access links to recommended websites, education, training, and other resources for general practices delivering palliative care including:
- Clinician Assist WA palliative care clinical pathways
- CareSearch evidence-based information and resources for general practice
- WA Health End of Life Care Program
To learn more about palliative care and advance care planning, contact Practice Assist on 1800 2 ASSIST (1800 2 277 478 or 08 6278 7900) or email practiceassist@wapha.org.au to connect with the Greater Choices for At Home Palliative Care team.

Ask Me Anything… GPACI Quarter 4 Payments
Presented by AAPM
20 May 2025 (10:30am to 11:30am AWST)
AAPM in collaboration with Services Australia, is excited to host a series of informative and interactive webinars called “Ask Me Anything”.
Some practices will have patients for the first time in Quarter 4, specifically, those who had the Incentive added to their MyMedicare profile in the July – September 2024 quarter. To receive the Quarter 4 payment, practices and providers must meet additional annual servicing requirements.
This session will provide an opportunity for you to learn and ask questions regarding the servicing requirements for the General Practice in Aged Care Incentive (GPACI).
This webinar will also discuss the requirements for Quarters 1 to 3 and have a more detailed discussion on the servicing requirements for Quarter 4.
Registration
This webinar is free for AAPM members and non-members.
Webinar Series: Dementia Demystified
Dementia Training Australia Education Sessions
22 May 2025 (12pm to 1pm) Webinar 1
Join us for a series of three webinars where Dementia Training Australia’s expert medical education team will discuss the recognition, diagnosis and post diagnostic management of a patient with dementia.
The Dementia Demystified webinar series will provide a practical and stepwise approach to improving knowledge, skills and confidence in dementia recognition, diagnosis and management within the general practice setting.
The webinars are designed for GPs, however general practice nurses and primary care health professionals are also welcome to attend.
Each webinar is accredited for 1 RACGP EA CPD hour.
Webinar 1: Trajectory of Dementia and Cognitive Impairment
- Recognise features of dementia and cognitive impairment.
- Explain the trajectory of dementia and cognitive impairment.
Find out more and register today.
Webinar: Accreditation for Nurses in General Practice
Presented by WA Primary Health Alliance
18 June 2025 (12pm to 1pm)
Join us for an informative and engaging webinar designed specifically for nurses working in general practice.
This session will cover the essential aspects of accreditation, including the latest standards, best practices and practical tips to ensure your team feels confident in demonstrating quality improvement to maintain the RACGP standards.
Key topics:
- The role of quality improvement in accreditation.
- Understanding accreditation standards and requirements.
- Best practices for maintaining compliance.
- The role of practice nurses in achieving accreditation standards.
- Practical strategies to support accreditation readiness.
- Insights from industry experts on accreditation best practices.
- Q&A session with industry experts.
Find out more and register today.
Webinar Series: Advancing Multidisciplinary Team Care in General Practice
Presented by WA Primary Health Alliance in partnership with AGPAL
3 June 2025 (1pm to 2pm) and 17 June (12pm to 1pm) Online

As general practice in Western Australia adapts to ongoing funding reform and increasing complexity in patient needs, this two-part interactive webinar series offers timely, targeted support for teams delivering multidisciplinary team (MDT)-based care.
Whether you’re a GP, nurse, allied health professional, practice manager or support staff, these CPD-accredited webinars will provide practical tools and strategies to enhance coordination, efficiency and equitable outcomes for all patients.
Each webinar is accredited for 1 RACGP EA CPD hour and includes an expert-led presentation, real-world case studies and a live Q&A segment to deepen understanding and facilitate application to your own practice.
Join us to strengthen your team’s capability and stay ahead of system reform.
To find out more, view the flyer and register for webinar 1 and webinar 2 today.
Hepatitis C treatment and the role of the GP
Presented by RACGP and WA Health
28 May 2025 (7pm to 8pm AWST) Online
Hepatitis C virus (HCV) infection continues to result in significant morbidity and mortality in Australia. Even with direct-acting antivirals, eradication of HCV remains a challenge with many patients unaware of their infection.
This webinar explores the GP’s role in treating HCV including:
- Identifying at risk populations
- Appropriate screening and testing
- Signs and symptoms
- Managing patients, surveillance and follow-up
- When to refer, and;
- What’s new in this space
You’ll have the opportunity to ask questions during the Q&A. If you have a question prior, you can submit it upon registration. Presented by Dr Jessamy Stirling and Dr Yolande Knight. Hosted by RACGP WA Co-Deputy Chair and GP Dr Mariam Bahemia.
This webinar is delivered in partnership with WA Health.
Aboriginal cultural diversity training – free online training for all practice staff
Presented by WA Primary Health Alliance
Available until June 2025

To help improve health outcomes for Aboriginal people, WA Primary Health Alliance (WAPHA) is offering free online Aboriginal cultural diversity training for all general practice staff.
The free online training is the SBS Inclusion Program (First Nations) that includes short learning modules, which take approximately an hour to complete in total, with the following learning outcomes:
- Improving knowledge about the history of Aboriginal culture and experiences.
- Understanding how to identify myths versus facts. Comprehending some of the stereotypes and assumptions sometimes made about Aboriginal people.
- Recognising the importance of spirituality in Aboriginal culture.
- Recognising the importance of family and kinship in Aboriginal culture.
- Grasping the impact of colonisation on Aboriginal people.
- Comprehending the trauma felt by the Stolen Generations and the intergenerational trauma still being felt today.
- Implementing tools to actively participate in the reconciliation process as both an individual and a business.
- Explaining what the Uluru Statement from the Heart is and how it came about.
- Describing the events that led to the referendum in 2023, which proposed Aboriginal people be recognised in an enshrined Voice to Parliament.
To find out more view the flyer here and register today!
Register now for a Clinician Assist WA live demonstration
Presented by Clinician Assist WA
Multiple Times & Dates Online

Clinician Assist WA is a secure website providing GPs and other health professionals with guidance for assessing, managing and referring patients across Western Australia. It has replaced HealthPathways WA, offering the same trusted local guidance, features and functionality and remains available at no cost.
The Clinician Assist WA team will run online demonstrations facilitated by a GP Clinical Editor throughout 2025 to support users. These sessions will demonstrate how to maximise integration of Clinician Assist WA into your clinical practice. Learn key functionalities of the website and how to access condition specific tools and resources, Referral Access Criteria (RAC) (where available), GPbook Specialist Directory and visiting specialist rosters.
Sessions have been approved for 1 CPD Educational Hour with RACGP and will be held online on the following dates:
- Thursday 12 June 2025 – 12:30pm to 1:15pm
- Wednesday 17 September 2025 – 12:30pm to 1:15pm
- Tuesday 18 November 2025 – 12:30pm to 1:15pm
Demonstrations are open to general practitioners, general practice staff and other health professionals registered to practice in WA.
Other Webinars, Events & Workshops
| Contraceptive Implant Theory Workshop Presented by SHQ 19 May |
| BreastScreen WA visit to Bruce Rock Presented by BreastScreen WA 19 May to 22 May |
| Advanced Training in Suicide Prevention Presented by Black Dog Institute 21 May |
| Behind the Frontline – How TEN Supports Health Professionals at Risk of Burnout Presented by Black Dog Institute 22 May |
| BreastScreen WA visit to Quairading Presented by BreastScreen WA 29 May to 30 May |
| C the Whole Story Forum III: Advancing Integration of Hepatitis C Care Presented by ASHM 29 May |
| Advanced HIV Nursing Course Presented by ASHM 30 May |
| WA Hepatitis B s100 Prescriber Course Presented by ASHM 3 June (Part 1) 10 June (Part 2) 17 June (Part 3) |
| BreastScreen WA visit to Cunderdin Presented by BreastScreen WA 3 June to 9 June |
| BreastScreen WA visit to Kellerberrin Presented by BreastScreen WA 10 June to 17 June |
| Wesley LifeForce Suicide Prevention Training Primary Care Support Staff Workshop (Subiaco) Presented by Wesley LifeForce 10 June |
| Unintended Pregnancy Counselling Training (webinar) Presented by SHQ 10 June to 11 June |
| MPA/MIA Melanoma Community Information Series (Tuesday evenings from 10-24 June) Presented by Melanoma Institute Australia 10 June to 24 June |
| Al in Mental Health: Navigating the Future of Clinical Practice Presented by Black Dog Institute 12 June |
| 2025 NU-CUES Training Dates Presented by CliniKids 17 June and 24 June |
| Talking About Suicide in Practice (3 hour interactive webinar) Presented by Black Dog Institute 17 June |
| Online education – Sepsis in Primary Care (webinar) Presented by Australian Commission on Safety and Quality in Health Care 18 June |
| Wesley LifeForce Suicide Prevention Training Primary Care Support Staff Workshop (Success) Presented by Wesley LifeForce 25 June |
| FPAA Certificate in Reproductive and Sexual Health for Doctors Presented by SHQ 30 June to 4 July |
| Course in Wound Closure Presented by Benchmarque Group 11 July |
| WA HIV Prescriber Update – ARV Update Presented by ASHM 15 July |
| WA HIV Prescriber Update – HIV and the Heart & Mind Presented by ASHM 29 July |
| ACNP National Conference Presented by Australian College of Nurse Practitioners (ACNP) 29 October to 31 October |
Acknowledgement
WA Primary Health Alliance acknowledges and pays respect to the Traditional Owners and Elders of this country and recognises the significant importance of their cultural heritage, values and beliefs and how these contribute to the positive health and wellbeing of the whole community.