Issue 233 – 13 November 2025

| Welcome to Practice Connect, a fortnightly update for practice managers, principals, nurses and administration staff on relevant issues, upcoming events and education. |

Medicare updates from November 2025

From 1 November 2025, a range of updates and modifications have been implemented to the Medicare Benefits Schedule.
1. Expanded eligibility for Bulk Billing Incentives (BBI), to include all Medicare-eligible patients.
- All Medicare-eligible patients are now eligible for bulk billing incentives, not just children and concession card holders.
- A triple bulk billing incentive can be claimed with face-to-face level B, C, D and E general attendance items, and level B video and phone general attendance.
- A single bulk billing incentive item can be claimed with other bulk billed unreferred general practice services such as antenatal care, mental health services, chronic condition management and health assessment items. For more information click here.
- Click here to download the factsheet.
- Information on MBS Online about Bulk Billing Incentives can be found here.
2. The Bulk Billing Practice Incentive Program (BBPIP) starts.
The BBPIP provides an additional quarterly incentive payment of 12.5% of MBS benefits for eligible services. The payment is split 50/50 between the doctor and the practice.
- Practices must register for MyMedicare to participate in BBPIP.
- See newly released Bulk Billing Practice Incentive Program Guidelines.
- Updated BBPIP signage requirements.
- How to register for BBPIP in Health Professional Services Online (HPOS), including how to view your BBPIP payment assessment and details.
- Infographic on key steps for practices to register and participate in BBPIP.
- Download the Frequently Asked Questions for practices and GPs document.
- The practice must bulk bill every eligible service for every Medicare-eligible patient.
- Eligible services are listed here Bulk Billing Practice Incentive Program: Eligible services.
- Access the Bulk Billing Incentives Calculator.
- View the new BBPIP Practice Readiness Checklist.
- Download the new BBPIP Planning Kit for general practice, including planning templates and Practice Readiness Checklist.
- Additional resources to support your practice when discussing bulk billing with patients including:
- RACGP Resources:
3. Changes to Mental Health item numbers under Better Access redesign.
- Download the Better Access redesign document.
- The Better Access Mental Health MBS User Guide provides examples of how to use relevant MBS items to meet the requirements of the Better Access Initiative, including links to the MBS items and MBS Online explanatory notes.
- A Medicare benefit will be payable for MHTP preparation, referrals for treatment services and reviews of a MHTP when a patient has seen:
- a GP or PMP at the general practice in which the patient is enrolled in MyMedicare, or
- regardless of whether the patient is enrolled in MyMedicare, by the patient’s usual medical practitioner.
- These requirements do not affect patients who have been referred via a Psychiatrist Assessment and Management Plan or by a direct referral from an eligible psychiatrist or eligible paediatrician.
- GP and PMP MHTP review items (2712, 92114, 92126, 277, 92120, and 92132) and GP and PMP ongoing mental health consultation items (2713, 92115, 92127, 279, 92121 and 92133) will be removed from the MBS.
- Further details can be viewed at MBS Online – Better Access changes from 1 November 2025.
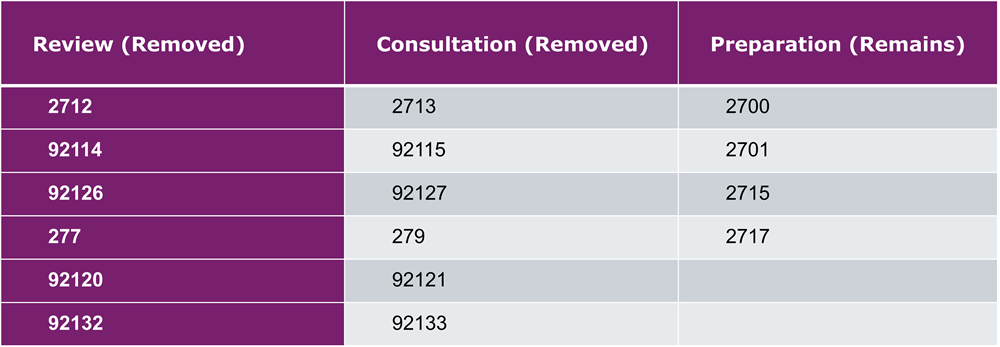
Key points:
- Removal of the 12 review and mental health consultation items provides GPs and PMPs greater flexibility to use the most appropriate time-tiered professional (general) attendance item, reflecting the time spent with patients. This includes items for longer consultations and, where applicable, the triple bulk billing incentive to review MHTPs and deliver mental health care and support to patients.
- Any MHTP referral dated prior to 1 November 2025 will remain valid until all treatment services specified in the referral (within the maximum session limit for the course of treatment) have been delivered to the patient.
- The MyMedicare and usual medical practitioner requirements will also apply to GP/PMP telehealth items for MHTPs, with these services no longer exempt from the established clinical relationship rule. Further information on the GP MBS telehealth (video and phone) established clinical relationship criteria and exemptions will be available from 1 November 2025 in explanatory note AN.1.1 on MBS Online.
- New Fact Sheets are available on the Department of Health, Disabilities and Ageing webpage here:
- Better Access Initiative resource collection | Australian Government Department of Health, Disability and Ageing
- Better Access fact sheet – patients | Australian Government Department of Health, Disability and Ageing
- Better Access – Involving family or carers in my mental health treatment | Australian Government Department of Health, Disability and Ageing
- Better Access fact sheet – professionals | Australian Government Department of Health, Disability and Ageing
- Better Access Telehealth frequently asked questions | Australian Government Department of Health, Disability and Ageing
- Better Access Cessation of the additional 10 sessions | Australian Government Department of Health, Disability and Ageing
- Better Access Initiative FAQs has been updated here.
- These changes to do not affect focussed psychological strategies which can continue to be available to any patient from any eligible GP and eligible PMP who has the appropriate training recognised by the General Practice Mental Health Standards Collaboration.
- Treatment services referred to under the Better Access Initiative are for patients who require at least a moderate level of mental health support. Information on other free or low-cost Commonwealth funded mental health treatment services can be found at: Medicare Mental Health or Mental Health in General Practice for referral options in your region or to learn more about the Stepped Care Model.
4. Increased rebates for Long-Acting Reversible Contraception.
- Insertion of an IUD (item 35503) from $93.55 to $215.95
- Removal of an IUD under general anaesthesia (item 35506) from $62.60 to $134.45
- Implantation of hormonal implants such as Implanon (item 14206) from $41.50 to $100.40
- Removal of Implanon (item 30062) from $70.85 to $105.15
5. Information about the MBS Telehealth arrangements.
- Ongoing MBS telehealth arrangements remain in place, providing a wide range of telephone and video services by qualified health practitioners to support safe and equitable access to telehealth services.
- For most patients eligibility for Telehealth services is now either an established clinical relationship where at least one face to face MBS service has occurred within the preceding 12 months OR the patient is registered with the provider and practice for MyMedicare. Some exceptions to these eligibility requirements apply.
- Further information and factsheets are available here.
6. Updated General Practice in Aged Care Incentive (GPACI) guidelines and Health Professional Education Resources are available.
There will be a delay in the 1 July – 30 September 2025 quarter payment, which was due by the end of October. The Department expect payments will be made in mid-November. Please see “12-month exclusion period removed” below for more details on the reason for this delay.
- 12-month exclusion period removed
- The Department has removed the exclusion period where responsible providers did not meet the 12-month care plan eligibility requirements for payment.
- Previously, if a patient did not receive two care planning services by the end of the 12-month period and a care planning service was not subsequently provided in the next quarter, the practice and provider would be ineligible for GPACI payments for that patient for the remainder of the patient’s new 12-month period.
- To ensure this change is reflected in the 1 July-September 2025 quarter payment and assessment, this payment will be delayed until mid-November. This ensures that providers can continue to confidently provide services to their GPACI patients.
- The GPACI Guidelines have now been updated.
- New GPACI hints & tips document is available.
- Further information on the changes and updates will be emailed to practices soon.
View the RACGP Changes to Medicare webinar series here.
You can find a full list of the 1 November 2025 changes here.
For information or support on the Medicare changes or MyMedicare please contact the Practice Assist Help Desk on 08 6278 7900 or via email practiceassist@wapha.org.au

Primary Sense in practice: QI bites and clinical insights
Welcome to Primary Sense in practice, a series of short, practical videos developed for health care professionals.
In this video, we’ll show you how to use and understand Primary Sense reports to establish and enhance quality improvement activities, so you can make informed data-driven decisions in your everyday practice.
For more information and to discover how the quality improvement team at WA Primary Health Alliance can help, visit Practice Assist or contact qi@wapha.org.au
Prepare your practice for the effects of heatwaves in your communities

Western Australia can expect a hot and dry summer this year, posing a risk to the health of patients in your community. Heatwaves have become an increasingly prevalent threat in Australia, with over half of heatwave-related deaths occurring in disadvantaged areas, where residents often lack access to adequate cooling infrastructure, and face additional health risks due to socioeconomic factors.
General practice has a role to play in preparing patients for the effects of heatwaves and can help to reduce the impact to communities.
Who is most at risk?
- Children, older people, pregnant women, people experiencing homelessness and those living with a disability.
- Patients living with chronic conditions and/or on multiple medications.
- Patients who are unable to adapt due to dementia, disability, substance abuse, pregnancy, breastfeeding or other factors.
- Those impacted by environmental factors e.g., outdoor workers.
- Aboriginal population living in remote areas.
Encourage your patients to prepare:
- Encourage vulnerable patients to plan check-ins with family during heatwaves to ensure support.
- Utilise bulk text message alerts to notify patients of predicted heatwaves, extreme heat events.
- Advise eligible patients about the Thermoregulatory Dysfunction Energy Subsidy to offset energy costs for controlling the temperature in their home.
- Recommend patients maintain hydration throughout the day and avoid unnecessary physical activity.
- Use air-conditioning and/or fans if available or go to publicly available air-conditioned places, such as libraries or shopping centres.
- Ensure patients have a back-up plan if essential medical equipment is reliant on electricity.
- Recommend that patients are utilising digital health tools such as My Health Record, which can assist patient care during emergency situations.
For up to date information, see below resources:
- Department of Health – Extreme heat and heatwaves and be prepared for extreme heat
- Emergency WA – Emergency warnings for Western Australia
- Bureau of Meteorology – Heatwave Service for Australia
- ABC Emergency – Live updates via internet and radio
Access the Primary Care Heatwave Plan:
Transition of WA Diabetes Patients to Adult Services – Primary Care Survey
This survey is intended for health professionals working in a primary care, community-based or private care setting.
For health professionals working in a paediatric public hospital service, please complete the paediatric service provider survey Paediatric Service Provider Survey.
For health professionals working in an adult public hospital service, please complete the adult service provider survey Adult Service Provider Survey.
When you have finished the survey, please press the SUBMIT button at the bottom of the last page.
The survey is estimated to take 10-15 minutes to complete. If the survey takes you over 30 minutes, it can be logged as Continuous Professional Development hours. This consultation will close Tuesday 18 November 2025.
Using quality improvement to boost the uptake of eScripts and Active Script Lists
To increase electronic prescribing (eScripts) and reduce paper prescribing, Shenton Park General Practice completed a quality improvement (QI) activity led by Sarah Reely, Practice Manager, with support from Chloe Morris, Practice QI Coach at WA Primary Health Alliance (WAPHA).
“Over the three-month activity, we surpassed our initial target of a 10% increase in eScripts, and eScripts are now the dominant method of prescribing at the practice. We’ve also had a surprising uptake of eScripts by older patients because they can use an Active Script List (ASL) to access all their active prescriptions at any participating pharmacy,” Ms Reely said.
The practice’s QI activity included adding an agenda item in clinical meetings about eScripts and ASL, championing the benefits to the practice team, and updating the resources in the waiting room to raise patient awareness.
“The increased use of eScripts and ASL has resulted in a range of benefits including improved workflow and efficiency for GPs and admin, improved environmental sustainability due to reduction in paper records, a reduction in lost prescriptions and increased patient satisfaction,” Ms Reely said.
If you would like assistance with developing a QI activity to boost the use of eScripts in your practice, refer to the eScript Plan-Do-Study-Act (PDSA) PDF or Word document or email WAPHA’s QI team via QI@wapha.org.au
For further information about eScripts and ASL, visit the Australian Digital Health Agency website or call Practice Assist on 08 6278 7900 or email practiceassist@wapha.org.au
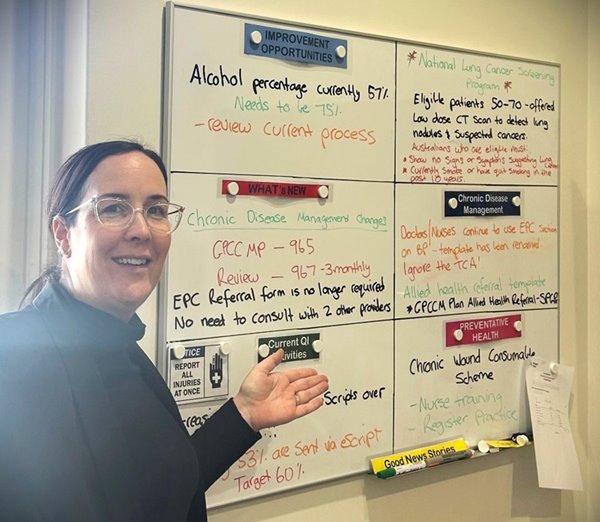
Sarah Reely, Practice Manager at Shenton Park General Practice.
Connected care: digital health across aged care
Currently, 43% of residential aged care homes are connected to My Health Record. The aim is to have 100% of residential aged care homes nationally connected.
Do all of your residents within the aged care homes you service have a shared health summary available to clinical staff?
Each year many older Australians enter aged care residential homes. When digital health services are connected, health care providers and authorised residential aged care staff have immediate access to a resident’s key health information, supporting greater continuity of care. Now 43% of residential aged care homes are connected, enabling them to access shared health summaries within My Health Record, a capability that was previously unavailable to them.
See WA Primary Health Alliance’s MHR Usage Clinical Considerations Guide for more information about using My Health Record and shared health summaries in general practice or contact Practice Assist.


Paid online focus groups on My Health Record
My Health Record enables key health information to be shared with all health care providers involved in an individual’s care across their entire health and aged care journey. Australians will soon experience better and faster access to their key health information in My Health Record. Read our recent Practice Connect newsletter for more information and how to prepare for these changes.
WAPHA’s Digital Health Team is seeking primary care providers to participate in a paid online (Microsoft Teams) focus groups to understand the benefits, barriers and challenges with accessing relevant health information and uploading records to My Health Record. This feedback will inform our approach to activities to support increased My Health Record adoption.
General practitioners:
- Tuesday 25 November 6:00pm – 7:30pm
- Thursday 27 November 6:00pm – 7:30pm
Practice nurses:
- Thursday 20 November 5:30pm – 7:00pm
- Monday 24 November 11:30am – 1:00pm
Practice managers:
- Friday 28 November 11:30am – 1:00pm
As there are only a limited number of places available, we will operate on a first in principle. Participants will be remunerated in line with WAPHA’s paid participation policy.
Contact the digital health team at digital.health@wapha.org.au for more information or find information and resources on My Health Record in the Digital Health Toolkit.
Get ready for summer!

As we head towards summer and the weather heats up, an effective vaccine management protocol will ensure that you are ready before an event or issue occurs. Ensure that the following are in place and included in your protocol:
o All staff should be trained to manage vaccine storage and cold chain management effectively, to ensure that all cold chain issues are identified and addressed in a timely manner.
o Contact names and numbers are readily available for reporting:
– Cold chain breaches and/or data logger maintenance issues.
– Power failures.
– Back-up vaccine storage options are documented and tested.
o A suitably trained, designated person (e.g. staff member) is responsible for coordination of vaccine storage and implementation of protocols.
o A suitably trained back-up person is available to relieve the designated person when required.
Managing a Power Failure
The management of a power failure in your health service will depend on the cause of the power outage, whether prior notice was given and the time of day the outage occurs. Some power companies send letters or provide text message alerts prior to scheduled power outages to allow for necessary planning. Check with your power company to determine whether this service is available in your locality.
Back-up plans
Always have a back-up plan and alternative storage that can be used if a power failure occurs. This will allow vaccines to continue to be stored between the recommended temperatures of +2°C and +8°C, thereby minimising vaccine loss and disruption to your facility’s activities. Each immunisation facility must practice implementing its back-up plan, including packing vaccines into alternative storage, to ensure that the plan will work in a real power failure situation.
Please contact your local Public Health Unit for more information and support.
Influenza immunisation program 2026
All vaccine service providers have received an email from Vaccine Orders to your Onelink email address about a 2026 Free Flu Program.
Please ensure you read and understand that the information in the email is EMBARGOED and should not be discussed until a formal announcement is made.
Declining adolescent immunisation rates
In recent years, adolescent vaccination coverage rates have declined. This exposes adolescents to risks and complications associated with vaccine-preventable diseases, including human papillomavirus (HPV), pertussis, and meningococcal disease.
Adolescents are eligible to receive one dose of each of the following National Immunisation Program (NIP)-funded vaccines:
- HPV and dTpa (diphtheria, tetanus, pertussis) in year 7
- MenACWY in year 10.
In WA, adolescent vaccines are primarily delivered via the School-based Immunisation Program. If vaccination at school has been missed, young people remain eligible for catch-up until the age of 20 for dTpa and MenACWY, and 26 for HPV.
WA Health is urging all immunisation providers to:
- Review immunisation records and use reminder or recall systems for patients who may be overdue for their age-appropriate vaccines
- Discuss adolescent immunisation with teens and their parents
- Offer opportunistic vaccination to eligible individuals.
Pertussis surge
Western Australia is experiencing a surge in pertussis (whooping cough) cases.
Whooping cough can be fatal in infants and can cause serious illness in older children and adults.
Providers are encouraged to check if patients are up to date with whooping cough vaccination and to highlight the importance of adult, pregnancy and childhood protection.
See the WA Immunisation schedule and Australian Immunisation Handbook for detailed information.
Changes to Immunisation Handbook chapters
Minor updates to several Australian Immunisation Handbook sections were actioned recently.
- Diphtheria, Pertussis (whooping cough), Poliomyelitis, Tetanus
Now includes advice that diphtheria-toxoid vaccines can be co-administered with immunisation products such as RSV monoclonal antibodies. - Infants exposed to immunosuppressive therapy in utero or through breastmilk
Gives more detailed guidance on live vs non-live vaccines, and specific advice for anti-CD20 therapies. - Preparing for vaccination
Includes an option for carrying adrenaline devices for underlying immunological disorders in the Pre-vaccination screening checklist.In addition, the Components of immunisation products used in Australia table has been updated to remove the meningococcal vaccine Menveo from the list of vaccines containing latex in their packaging and provides detail on which packaging components contain latex. - Vaccination for people who are immunocompromised
Updates to Types of medical conditions and immunosuppressive therapy and associated levels of immunocompromise table regarding mTOR inhibitors and Immunosuppressive potential of small molecule targeted therapies table regarding ALK inhibitors and CDK inhibitors.
Minor changes were also made to listings for the disease chapters for measles, varicella (chickenpox), tuberculosis and Q fever.
November is Pancreatic Cancer Awareness Month

Pancreatic cancer occurs when abnormal cells in the pancreas grow out of control. Several types of growths (or “tumours”) can occur in the pancreas. Some of these growths may be cancerous, while others may be non-cancerous. Cancerous tumours can occur on any part of the pancreas, including the head, body or tail of the organ.
Pancreatic cancer can be difficult to detect due to the location of the pancreas. Symptoms are often vague and can be similar to other medical conditions.
Pancare Foundation offer a referral service for patients diagnosed with an upper gastrointestinal cancer who could benefit from contact with their team of specialist upper GI cancer nurses, counsellors and care navigators. The referral can be accessed here.
Health professional resources and information are available here.
A range of resources is also available, access here.
National Cancer Screening Register

The National Cancer Screening Register (NCSR) is a digital platform that supports, facilitates and streamlines engagement in the National Bowel Cancer Screening Program, National Cervical Screening Program, and National Lung Cancer Screening Program for eligible participants and their health care providers.
The NCSR provides a single electronic record for each participant and delivers a secure, national infrastructure for collecting, storing, analysing and reporting screening data.
Health care providers can access participants cancer screening information and manage participation in the bowel, cervical, and lung cancer screening programs through secure online portals and integrated clinical software.
Clinical software integration
Integration is designed to streamline workflows for health care organisations, allowing you to access and report patient clinical information for the bowel, cervical and lung cancer screening programs directly from the software you use every day.
Health care organisations using integrated software can:
- Support patient participation: Access patient bowel, cervical and lung cancer screening information and status (including overdue and follow-up alerts), and enrol patients in the National Lung Cancer Screening Program.
- View and submit screening results: Including colonoscopy, colposcopy findings or radiology reports, ensuring accurate program participation.
- Order bowel screening program test kits: Directly to a patient’s address or record when you have issued one to a patient during a consultation as part of the alternative access to kits model (bulk orders are made through the Health care Provider Portal).
- Verify and update patient contact details and demographic information.
- View screening program-related correspondence: Stay updated with program communications to track your patient’s screening journey.
- Nominate health care providers or personal representatives: Assign a health care provider or personal representative to ensure comprehensive patient care.
Currently integration can be done with the following software: BP Premier, Communicare, Medical Director and MMEx.
To learn more about integration, access here.
New Learning Management System (LMS) for online immunisation modules
The WA Health online immunisation education modules are now on a new Learning Management System (LMS) platform, Reach360.
Existing user accounts have been automatically transferred and no action is required by existing active users. New users, or users who have not accessed the LMS for over 30 days, can register using the new LMS link in WA Health modules and registration to access the online modules.
For more information about education requirements and for further instructions to use the immunisation education online modules, please see the Immunisation education (health.wa.gov.au) webpage.
Eliminating Cervical Cancer Conference 2025
Presented by Immunisation Coalition
17 November 2025 (9am to 12 noon AWST)
Hosted by the NHMRC Centre for Excellence in Cervical Cancer Control, the Eliminating Cervical Cancer Conference will be a virtual event on the inaugural World Cervical Cancer Elimination Day.
ECC2025 will bring together leading experts, researchers, and health care professionals to discuss and advance the mission of eliminating cervical cancer.
The theme for ECC2025 is Working towards Elimination: Success, Innovation and Challenges in Implementation. This conference will feature:
- Panel Discussions: Engage with thought leaders as they explore the successes, innovations, and challenges in implementing cervical cancer elimination strategies across the region.
- Showcase of C4 Funded Research: Highlighting equity-focused initiatives, meaningful consumer and community engagement, and innovative data systems that enable targeted, impactful approaches—demonstrating the transformative outcomes of C4-funded projects in action.
For further information and to register, click here.
Shingles update
Presented by Immunisation Coalition
19 November 2025 (3pm to 4pm AWST)
This Immunisation Coalition webinar on Shingles completes a suite of 7 infectious diseases webinars.
Professor John Litt will provide an update on shingles epidemiology, revisit eligibility criteria including immunocompromised individuals and risk categories, disease burden and current trends in vaccination rates.
To register and for further information, click here.
Changes to the WA Immunisation Schedule Lunchtime webinar
Presented by Communicable Disease Control Directorate (CDCD)
20 November 2025 (1pm to 2pm AWST)
The Communicable Disease Control Directorate (CDCD) Immunisation Program is hosting a webinar covering important changes to the WA Immunisation Schedule.
This session will focus on updates related to pneumococcal and RSV vaccines. Attendees will gain insights into the rationale behind the changes and implications for immunisation providers.
Presenters for this event will be Professor Paul Effler, Senior Medical Advisor, CDCD and Professor Chris Blyth, Paediatric Infectious diseases Physician and Clinical Microbiologist, The Kids Research Institute Australia.
Questions you’d like addressed during the Q&A need to be submitted in advance via this Survey Link by 4pm, Thursday 13 November.
Enhancing men’s and women’s health in primary care
Presented by WA Primary Health Alliance
19 November 2025 (12pm to 1pm)
Join us for a practical and engaging quality improvement (QI) webinar designed to support primary care professionals with delivering gender-responsive health care.
This webinar will cover the following topics:
- Understanding QI
- Data-driven decision making
- Gender-specific health issues
- Primary care led initiatives
- Health promotion
- Further education
To find out more, view the flyer and register today.
Register now for a Clinician Assist WA live demonstration
Presented by Clinician Assist WA
Tuesday 18 November – 12:30pm to 1:15pm

Clinician Assist WA is a secure website providing GPs and other health professionals with guidance for assessing, managing and referring patients across Western Australia. It has replaced HealthPathways WA, offering the same trusted local guidance, features and functionality and remains available at no cost.
The Clinician Assist WA team will run online demonstrations facilitated by a GP Clinical Editor throughout 2025 to support users. These sessions will demonstrate how to maximise integration of Clinician Assist WA into your clinical practice. Learn key functionalities of the website and how to access condition specific tools and resources, Referral Access Criteria (RAC) (where available), GPbook Specialist Directory and visiting specialist rosters.
Sessions have been approved for 1 CPD Educational Hour with RACGP and will be held online. This will be the final live demonstration for 2025 with no further sessions planned for 2026. If you are interested, register now.
Demonstrations are open to general practitioners, general practice staff and other health professionals registered to practice in WA.
Immunisation and Cancer Screening Preventative Health Forum
Presented by WA Primary Health Alliance
26 November and 1 December 2025 (6pm to 9pm)

Join us for one of the Immunisation and Cancer Screening Preventative Health Forums in Perth South or Perth North.
These in-person events are designed to support practice nurses with understanding the National Immunisation Program (NIP), administering vaccinations and increasing cancer screening rates.
To find out more, view the flyer and register for the Perth South Forum or the Perth North Forum today.
Medico-legal considerations for GPs responding to family and domestic violence
Presented by WA Primary Health Alliance
29 November 2025 (8am to 10.30am) Aloft Rivervale – 1.5 RACGP EA hours
This WA Primary Health Alliance workshop invites GPs and supporting members of the practice team to strengthen their response to patients experiencing family and domestic violence (FDV) through best-practice documentation and collaborative care. A multidisciplinary panel from the Sexual Assault Resource Centre, MDA National, Women’s Legal Service and the Police FDV Response Team will share insights on medical and legal processes in responding to FDV.
Download the flyer or register here. Breakfast provided.
New and updated sexual health education from ASHM
Presented by ASHM
Ongoing learning module and webinar
Sexually transmissible infections (STI) cases are rising in Western Australia. Syphilis notifications in particular have risen dramatically, with a 32-fold increase in cases since 2005 reported by the Western Australian Department of Health. This year, syphilis has already caused two stillbirths in Western Australia.
It is vital that West Australian health care workers are up-to-date with the latest information on syphilis and other STIs. To support you, ASHM has recently launched two new or updated educational resources to strengthen STI testing and treatment, and to increase syphilis awareness in WA.
Online Learning Module, 1.5 CPD hours
This recently updated module reflects current WA guidelines and supports primary care clinicians to discuss sexual health with confidence, engage communities, and deliver STI screening, testing, treatment, and contact tracing.
Webinar highlights video, 0.5 CPD hours (self-claimed)
This highlight reel from a recent panel webinar covers effective methods to raise awareness about syphilis among both the general public and health care providers, sharing insights from recent educational campaigns and community engagement initiatives.
These activities are funded by the Western Australian Department of Health.
Other Webinars, Events & Workshops
Acknowledgement
WA Primary Health Alliance acknowledges and pays respect to the Traditional Owners and Elders of this country and recognises the significant importance of their cultural heritage, values and beliefs and how these contribute to the positive health and wellbeing of the whole community.







