Issue 234 – 27 November 2025

| Welcome to Practice Connect, a fortnightly update for practice managers, principals, nurses and administration staff on relevant issues, upcoming events and education. |

Year in Review 2024-2025: Strategic alignment, data-driven decision and collaborative partnerships

WA Primary Health Alliance (WAPHA) is proud to share our Year in Review 2024-2025, Activity Snapshot 2024-2025, and Cultural Competency, Equity and Inclusion Snapshot 2024-2025.
This year was defined by strategic alignment, collaborative partnerships, and a focus on inclusion and data-driven decision-making in the context of the ambitious Australian Government primary health care reform priorities.
Primary Health Networks work within a complex landscape of diverse stakeholders, often with competing priorities, in thin market areas where service delivery is challenging. Added to this is a rapidly evolving policy environment that demands strong leadership and a commitment to cultural change. Navigating this complexity, fostering collaboration, and bringing agencies and providers together, is central to how WAPHA is making a difference and delivering better health outcomes for Western Australians.
We thank our partners and member organisations, commissioned service providers and primary health care professionals for their continued trust and collaboration.
Enjoy the highlights in our Year in Review 2024-2025 as we reflect on our collective impact over the past year through integration, collaboration and innovation as we work towards achieving health equity.

Medicare updates from November 2025

From 1 November 2025, a range of updates and modifications have been implemented to the Medicare Benefits Schedule.
- Expanded eligibility for Bulk Billing Incentives (BBI), to include all Medicare-eligible patients.
- Introduction of the Bulk Billing Practice Incentive Program (BBPIP). Provides an additional quarterly incentive payment of 12.5% of MBS benefits for eligible services when the practice bulk bills all eligible services. The payment is split 50/50 between the doctor and the practice. Registration for the BBPIP requires the organisation to be registered for MyMedicare.
- Changes to Mental Health item numbers under Better Access Mental Health Treatment Plan redesign.
- Increased rebates for Long-Acting Reversible Contraception
- Telehealth service eligibility now linked to an established clinical relationship OR where a patient is registered for MyMedicare. This includes the eligibility for Nurse Practitioner telehealth.
- Updated General Practice in Aged Care Incentive (GPACI) guidelines and Health Professional Education Resources are available. Updates guidelines include the removal of the 12-month exclusion period.

See the AusDoc MBS quick guides MBS Quick Guide November 2025 and MBS Quick Guide Telehealth for details.
You can find a full list of the November 2025 changes here.
For further information on all of the above changes, plus resources to help you and your practice see the Practice Assist Medicare Changes November 2025 Factsheet, contact Practice Assist or your Primary Care Navigator.
Cheaper cancer and chronic conditions medicines now on PBS
The Australian Government Department of Health, Disability and Ageing has announced new additions to the Pharmaceutical Benefits Scheme:
- Daratumumab (Darzalex®) will be expanded for the treatment of multiple myeloma, a rare and complex blood cancer that originates in plasma cells.
- Brentuximab vedotin (Adcetris®) in combination with doxorubicin, vinblastine and dacarbazine, will be listed for the first time to treat patients with advanced Hodgkin lymphoma.
- Brexpiprazole (Rexulti®) will be expanded for the treatment of schizophrenia.
- Durvalumab in combination with Tremelimumab (Imfinzi® Imjudo®) will be listed for the first time for the treatment of advanced liver cancer.
- Iptacopan (Fabhalta®) will be listed for the first time for the treatment of Paroxysmal Nocturnal Hemoglobinuria.
- Palovarotene (Sohonos®) will be expanded to allow treatment of both ongoing symptoms and flare-ups in people with Fibrodysplasia Ossificans Progressiva.

Workshop on futureproofing your general practice
GPs and practice teams heard about practical strategies and tools, how their peers are implementing innovative ways of working, and guidance on embedding Strengthening Medicare measures that can help them improve patient care and operational sustainability.
Co-hosted by primary care innovation, policy and reform expert, Dr Walid Jammal, and internationally recognised expert in patient-centred medical homes and health care system transformation, Dr Kirsten Meisinger, the events attracted 121 attendees from across the state, reflecting the widespread interest in futureproofing general practice across WA.
The facilitators guided participants through the intention behind the reforms, what GPs can expect, and practical ways to adapt without compromising clinical outcomes.
Attendees also had the chance to hear global insights on evolving models of care, quality improvement, and sustainability in a shifting funding environment.
WAPHA regularly runs events and webinars aimed at general practice teams, so keep an eye out for more opportunities in our publications.
Watch the highlights of the workshop and hear participant feedback, here.

For information or support on Future proofing your practice please contact the Practice Assist Help Desk on 08 6278 7900 or via email practiceassist@wapha.org.au
View your My Practice Data Reports
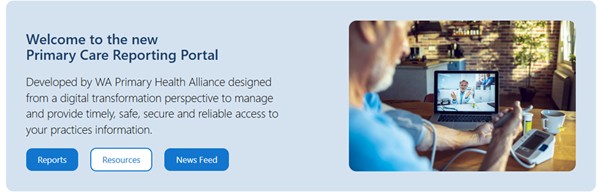
Have you logged into the Primary Care Reporting Portal (PCRP) to view your My Practice Data Reports if you have Primary Sense?
You can access the PCRP by logging in with your email address and email password, full instructions can be found in PCRP Manual For Practice Staff. Once logged in you will be able to view My Practice Data Reports and give other members of staff access, instructions for the reports can be found in My Practice Data Report User Guide.
The reports will give you a valuable insight into your practice data including the 10 Quality Improvement Measures activity, patient demographics, chronic conditions & mental health, cancer screening & health assessments, digital health and lifestyle risks.
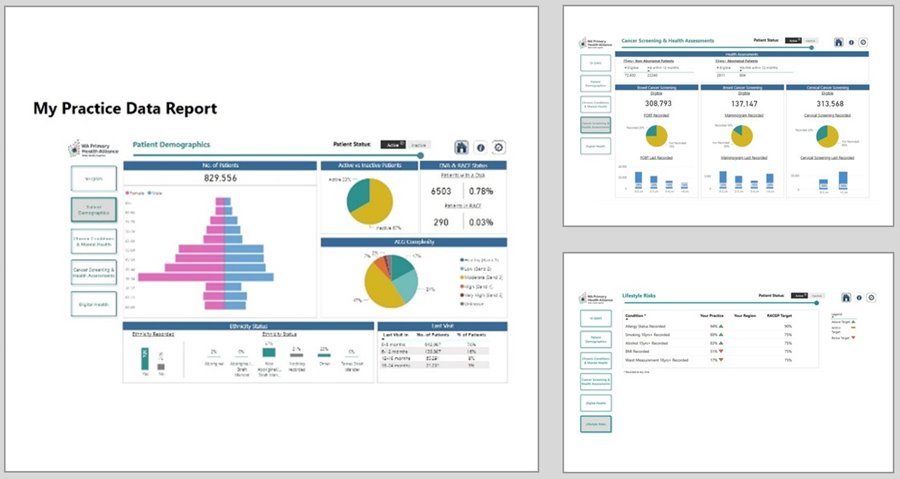
From the reports you can identify potential quality improvement activities and opportunities to improve patient outcomes.
For information or support with My Practice Data Reports, PCRP, or other support needs:
- Contact the Practice Assist Help Desk on 08 6278 7900 or via email practiceassist@wapha.org.au
- Book a Primary Care Navigator Practice Support meeting, click here
- For support with quality improvement activities in your practice, please contact the Primary Care Quality Improvement team via email at QI@wapha.org.au
- To help us keep in touch with your practice update your General Practice details, here
Practice Assist looking forward to 2026

WA Primary Health Alliances Practice Assist service has been providing support for general practices across WA since 2017.
Practice Assist encompasses all aspects of general practice support, and the free service can assist general practice teams with:
- phone support via phone – 08 6278 7900.
- email support via practiceassist@wapha.org.au
- support from local WA friendly and experienced staff
- support and information regarding digital health services
- connection to Quality Improvement Coaches and Primary Care Navigators
- a dedicated website with updates, information, resources and more
- an online Tool Kit of fact sheets, templates, checklists and guides
- a fortnightly eNewsletter, Practice Connect with industry news and updates
- education sessions, including webinars and workshops
Practice Assist will close for the holiday period from 25 December 2025 and reopen on 5 January 2026. From 5 January we will be making the following changes to our service:
- Operating hours will be from 8:30am to 4:30pm Monday to Friday excluding public holidays.
- Our phone number is changing to 08 6278 7900, with the 1800 number no longer in operation.
We look forward to continuing to support WA general practices in 2026.
Secure messaging improves referrals
More than 10 per cent of the referrals received are duplicates (submitted multiple times and/or via multiple methods). This contributes to delays in other referrals being processed as duplicate referrals must be checked to ensure they are not an amended referral containing new information.
A further 10 per cent of referrals are missing the information necessary for the CRS to be able to process the referrals. This may be due to missing pages or missing clinical information.
Secure messaging is the preferred and most reliable way to send referrals to the CRS and over 600 specialist providers across WA. Many of these providers, including the CRS, provide referral templates that automatically pull information from the patient record, saving time and minimising the risk of rejected referrals.
Additional benefits provided by secure messaging include:
- Maintains patient confidentiality
- Reduced administrative burden compared to fax or post
- Faster processing of referrals
- Visibility of referral acceptance
- Integration with existing clinical software
- Free to use for referring organisations
Secure message referrals can be sent to the CRS using HealthLink or MMEx.
Further information on secure messaging is available from the Australian Digital Health Agency or by contacting Practice Assist. For support on implementing or using secure messaging, contact your clinical software or secure messaging provider.
The new Aged Care Act and DVA funded care
The new Aged Care Act commenced on 1 November 2025 as part of the Australian Government’s commitment to creating a simpler, fairer and more respectful aged-care system.
If you are an existing provider of aged care services nothing will change the way you deliver Department of Veterans’ Affairs (DVA) funded care and support services to eligible veterans and war-widowed partners to help them live independently, safely and comfortably at home or in residential aged care.
For further information about what has changed with the new Aged Care Act, visit the DVA website or the My Aged Care website.
New quick guide about DVA funded supports for veterans with cognitive concerns
The Department of Veterans’ Affairs (DVA) has released a new quick guide to help general practitioners and other primary care providers understand what DVA supports are available for veterans with cognitive concerns.
The new two-page printable quick guide provides eligibility information for the investigation and treatment of cognitive concerns in veterans, and DVA funding arrangements.
For further information, email providerengagement@dva.gov.au
Annual payment available to patients for incontinence products
Incontinence is a chronic condition affecting one in three people over the age of 15. To help people manage their incontinence, the Australian Government’s Continence Aids Payment Scheme (CAPS) helps people experiencing incontinence with some of the costs of buying continence products.
The annual payment can be used by eligible patients to buy products from a supplier of their choice. The application includes a Health Report from a registered health professional Learn more about CAPS and how your patients can apply on the Department of Health Disability and Ageing website.
More continence resources GPs are available on the Continence Health Australia website.
Support older people to record preferences for Aboriginal and Torres Strait Islander assessment organisations
GPs can now register a patient’s preference for an aged care assessment with an Aboriginal and Torres Strait Islander assessment organisation. This is done through the HealthLink GP eReferral ‑ system.
Three Aboriginal and Torres Strait Islander aged care assessment organisations are now available in some regions across Australia.
For more information:
- Visit Aboriginal and Torres Strait Islander aged care assessment organisations
- Visit the My Aged Care website
- Call My Aged Care on 1800 200 422.
New resources to support children and families with attention, regulation and ADHD challenges
The Child Development Service in Perth has created a suite of new, online resources to provide consistent, evidence-based information to families who have concerns about their child’s attention, regulation and concentration skills, as well as to families who have a child with a confirmed diagnosis of ADHD.
Developed by clinicians with input from the community, including Aboriginal and multicultural families, these resources include lived experience of caregivers across topics including:
- Parent education: Ways to support attention, regulation and concentration
- School resources: Helping your child focus in the classroom
- Home resources: Developing healthy screen time habit
- ADHD resources: Talking about ADHD with your child.
Key resources have been translated into 10 languages.
This is part of a broader update of the Child Development Service webpages, which now provide clearer, more user-friendly information and resources to families who have concerns about their child’s development.
Bidi Wungen Kaat – St James Transitional Care Unit Prevention and Recover Program now open to patients state-wide
Bidi Wungen Kaat is now accepting GP referrals for eligible adults living anywhere in WA who require a step up from the community to manage their mental health where capacity allows.

The program provides an evidence-based, innovative approach to mental health care delivered by the East Metropolitan Health Service (EMHS) in St James, within the Town of Victoria Park. The 20-person Prevention and Recovery Unit is a sub-acute residential service providing contemporary staged recovery support for people experiencing complex emotional issues. Referral to the service should not be for medication adjustment or diagnostic clarification.
Please note that people in crisis or presenting as a risk to themselves or others, need to be assessed in an ED for assessment.
Bidi Wungen Kaat is a sub-acute step-up/step-down service which is not set up to provide crisis admissions, or support for people requiring an acute level of mental health care. Also, patients with acute medical needs may not be admitted to the unit as the unit is not equipped with emergency medication trolley and is not supported by acute medical care teams.
Read more about the service, programs and referral process in the November edition of GP Connect.
Supporting patients with changing their legal gender
A Statement in Support of Change of Sex or Gender is a simple but essential confirmation required by trans, gender diverse and non-binary (TGDNB) people to legally change their sex or gender in WA. In providing this documentation, GPs, psychiatrists and psychologists can play a vital role in affirming their patient’s identity and improving their access to accurate legal records.
These statements are only a confirmation that a patient has received appropriate clinical treatment in relation to their gender. The term ‘appropriate clinical treatment’ is not defined in WA legislation and is based on the individual needs and circumstances of the patient. There are no minimum requirements for the treatment.
Clinicians can refer to the information, brochures and example statement templates provided by the WA Registry of Births, Deaths and Marriages on WA.gov.au
- Information for doctors and psychologists about the process for adults to update their sex or gender in their birth registration
- Doctor or psychologist statement – adult patient
- Information for doctors and psychologists about the process for children (aged 12 to 17 years) to update their sex or gender in their birth registration
- Doctor or psychologist statement – child patient (aged 12 to17 years)
The Clinician Assist WA Transgender Health and Gender Diversity pathway provides advice on creating welcoming and inclusive clinical environments for TGDNB people, provides details on available supports for TGDNB people and their families, and outlines how to assess and manage TGDNB people of all ages. It also includes a section on professional support.
Transfolk WA has also developed a patient guide outlining each step in the process of applying to change legal gender, which can be shared during consultations.
Supporting your practice to be LGBTIQA+ inclusive
As part of our efforts to improve health equity, WA Primary Health Alliance (WAPHA) is actively involved in advocating for and facilitating safe, inclusive, and culturally appropriate primary care services for LGBTIQA+ people.
We know that social exclusion, discrimination, stigma and marginalisation are some of the issues experienced by LGBTIQA+ people accessing health care. Not only do these factors increase the risk of adverse impact on their health and mental health, but they also create barriers to accessing health and social care services.
General practice is well placed to influence the health and wellbeing of LGBTIQA+ people, and many practices are already effectively engaging with and treating their LGBTIQA+ patients in safe and welcoming practices.
If your practice would like to improve your understanding of the issues facing your LGBTIQA+ patients or you are seeking support with responding sensitively and effectively, see below for some helpful resources. You can also access more resources and information in the WA Primary Health Alliance LGBTIQA+ Toolkit*

Visual displays:
A simple yet effective way to show that your practice is LGBTIQA+ inclusive, is by displaying a welcoming sign or poster. Your practice can register for ACON’s Welcome Here project, a national initiative that enables organisations to register as a safe place for LGBTI people and provides supporting resources.
Clinician Assist WA Transgender Health and Diversity Health pathway:
Based on national and international guidelines, this pathway outlines the assessment, management and referral pathways to specialised services for trans, gender diverse and non-binary (TGDNB) people of all ages. It also provides advice on creating welcoming and inclusive clinical environments for TGDNB people and provides details on available supports for TGDNB people and their families.
Note: If you are not logged into Clinician Assist WA, clicking on the linked pathways in this article will automatically redirect you to the login page. To access the linked pathways, please log in to your Clinician Assist WA account and then click the link to the pathway within the article.
Learn more about inclusive LGBTIQA+ language:
Understanding and using the language and terminology associated with your LGBTIQA+ patients can help to ensure that services and practices are inclusive and respectful. Some helpful guides include:
- External Language Guide – ACON
- Misgendering + Pronouns – Wear it Purple
- WordsAtWork – Building inclusion through the power of language – Diversity Council Australia
- Inclusive Language Guidve – LGBTIQA+ Health Australia
Training in gender diversity and transgender health:
- LGBTIQA+ Diversity Workplace Training – Sexual Health Quarters
- Introduction to LGBTIQ – Inclusive Practice (online modules) – Rainbow Health
- Rainbow Network Training – Rainbow Health
- Webinar: Working with gender diverse people and their families – Australian Government Australian Institute of Family Services
- Aware workshops (formerly Opening Closets): Living Proud
* The WA Primary Health Alliance LGBTQA+ Toolkit has been compiled based on advice from our LGBTIQA+ stakeholders and is to be used as guidance only. It is at the discretion of users of the Toolkit to determine the suitability and currency of this Toolkit to meeting their needs.
For information or support on LGBTIQA+ inclusive please contact the Practice Assist Help Desk on 08 6278 7900 or via email practiceassist@wapha.org.au
Safer Options resources for inclusive care

In 2022 WAPHA contracted Curtin University and the WAAC to provide resources and recommendations for enhancing primary care responses to Intimate Partner Violence in LGBTIQA+ relationships. Their research found that half of the 523 participants had experienced one or more forms of abuse in an intimate relationship, and that most people reported difficulty accessing inclusive primary care services due to fear of judgement. Practitioners who identified as LGBTIQA+ were also interviewed and provided rich insights as to how care can be inclusive and safe.
The research highlighted the importance of visual cues for people in the LGBTIQA+ community to feel confident in trusting their health provider. Whilst many primary care providers are inclusive and welcoming, very few signal this visually in their clinics.
Free posters and brochures are now available to you to assist in this, thanks to the Safer Options project, as well as a website focused on primary care awareness and education.

WA Primary Health Alliance Palliative Care Champions Project – Request for Proposal (RFP) opening early December 2025
The Request for Proposal (RFP) to gain grant funding of $20,000 will be open at the beginning of December for the Palliative Care Champions Project. WA Primary Health Alliance (WAPHA) will be recruiting 15 general practices across WA to undertake this project which will commence in March 2025 and run for 12 months. The intention of this project is to strengthen current approaches to Advance Care planning and screening for unmet palliative care needs through routine health assessments and Chronic Disease Management care. WAPHA has successfully conducted this project with positive outcomes for the practices who participated.
For information WAPHAs Greater Choices for At Home Palliative Care program including the Palliative Care Champion project in general practice please visit WAPHA Palliative Care.

Australian Immunisation Register (AIR) policy: update to childhood pneumococcal schedule rule changes
Children who received their third dose of the pneumococcal vaccine before 11 months of age are now showing as overdue in the AIR for their 12-month pneumococcal booster vaccine. This is clinically correct and aligns with the recommendations in the National Immunisation Catch-up Calculator (NICC).
To address this, the catch-up schedule table in the Australian Immunisation Handbook has been updated to align with AIR rules and the NICC. Services Australia has issued letters to families whose children are now showing as ‘not up to date’ for their 12-month pneumococcal dose.
To minimise any potential impact on family assistance payments, an extension has been granted. Affected families now have until 31 December 2025 to ensure their child receives the recommended booster vaccine.
New and improved Immunisation Handbook app now available
The Australian Government Department of Health, Disability and Ageing has launched a new version of the Immunisation Handbook mobile application, available on the Apple App Store and Google Play.
This latest release delivers a faster, more responsive search experience, smoother browsing and bug fixes that resolve content update issues affecting some users.
The Immunisation Handbook app allows you to take the Handbook with you on your phone or tablet and easily access it when and where you need it – even if you are not connected to the internet.
Access for Apple devices.
Access for Android devices.
Reminder: free Japanese encephalitis vaccine available for those at risk
As we head into the warmer months, Australian health authorities are encouraging eligible people to take advantage of state and territory funded Japanese encephalitis (JE) vaccination programs.
JE, a rare but potentially fatal disease, has been detected across multiple regions across Australia since 2022, prompting targeted immunisation efforts.
Free vaccines are offered in the Australian Capital Territory, New South Wales, Victoria, South Australia, Queensland and Western Australia to eligible people who are at high risk of JE virus infection.
As it takes up to four weeks to develop immunity, timely vaccination is encouraged.
Introduction of the New Aged Care Act: key messages for COVID-19 vaccination
With the introduction of the new Aged Care Act 2024 on 1 November 2025 and end of year fast approaching, the Department of Health Disability and Ageing has prepared key messaging to:
- increase awareness and encourage COVID-19 vaccinations in aged care ahead of the festive season.
- increase awareness and understanding of residential aged care provider obligations to provide vaccine access for residents and staff.
To ensure clear and consistent messaging, please share the following when advising or preparing your own communications with your patients and the aged care sector.
Key Messages
Vaccines are the best protection of serious illness and hospitalisation in older people. From 1 November 2025, the new Aged Care Act 2024 strengthened the requirement for residential aged care providers to provide access to recommended vaccinations for their residents. This includes vaccines such as influenza, COVID-19, shingles and pneumococcal.
The Western Australia Immunisation schedule outlines which vaccines an individual is eligible to receive for free in WA and when.
As we approach the festive season, it’s important to make sure aged care residents and staff keep up to date with their COVID-19 vaccination, as cases normally increase over this period. COVID-19 vaccines are free and recommended:
- every 6 months for people aged 75 and over
- every 12 months for people aged 65 to 74 and also aged care workers
- every 12 months for adults who are severely immunocompromised.
It is recommended to have the COVID-19 vaccine even if you’ve recently had COVID-19 disease.
Key messages for patients
Residential aged care homes are communal environments where infections can spread quickly.
Vaccination helps:
- minimise transmission of vaccine-preventable diseases
- protect residents, staff, visitors, and the broader community from vaccine preventable disease and their complications.
For more details, you can refer to the fact sheet COVID-19 vaccination information for residents of aged care homes.
You can use your immunisation history statement to see what immunisations you’ve had, as well as those that are due or overdue. Guidance on how to get your immunisation history statement is available at Services Australia.
For further information about the new Aged Care Act, please refer to the department’s website, by clicking here.
COVID-19 vaccines in Australia poster updated
The Australian Government Department of Health, Disability and Ageing has updated its ‘COVID-19 vaccines in Australia’ resource.
The A3 poster provides an overview of the COVID-19 vaccines currently approved under the National COVID-19 Vaccine Program.
It includes images of each vaccine vial along with details such as the vaccine name and type, approved age groups, dosage and storage requirements.
View the poster here.
World Cervical Cancer Elimination Day
On 17 November, countries around the world marked Cervical Cancer Elimination Day – an annual event to raise awareness of the importance of regular cervical cancer screening, accessible treatment services and the role human papillomavirus (HPV) vaccine can play in eliminating the disease.
The day supports the World Health Organization (WHO) global strategy to accelerate the elimination of cervical cancer as a public health problem by 2030.
The National Strategy for the Elimination of Cervical Cancer in Australia aligns with the WHO Strategy, setting national targets of:
- 90% of adolescents (including boys) vaccinated against HPV by 15 years of age
- 70% of women aged 25–74 years participating in cervical screening every 5 years
- 95% of those with cervical disease receiving optimal treatment for pre-cancer and cancer
- less than 4 new cases of cervical cancer for every 100,000 women.
With HPV vaccination coverage falling among Australian adolescents over the past five years, Cervical Cancer Elimination Day is also a timely reminder of the need to address coverage equity issues outlined in the National Health and Medical Research Council’s 2025 Cervical Cancer Elimination Report.
Access the report here.
National Cervical Screening Program monitoring report 2025
The latest monitoring report for National cervical screening was released on 17 November 2025.
This report presents statistics on the National Cervical Screening Program using key performance indicators to assess how well it is meeting its aim to reduce cervical cancer cases, illness, and deaths within Australia’s broader strategy to eliminate cervical cancer as a public health problem.
Key indicators show that from 2020 – 2024 over 5.5 million eligible participants had a HPV test. This equates to 77.9% of the target population and in 2024 only 7% of screening HPV tests were positive for HPV types that cause cervical cancer.
However, of the 1.8 million invitees aged between 25 – 74 in 2024, only 37.4% had a HPV test within 6 months and sadly 210 women died from cervical cancer in 2023.
To read the report in full, click here
To access resources and information about screening in WA, click here.
Immunisation education opportunities
As immunisation providers, staying informed and up-to-date on new research and innovations, current immunisation programs, the latest practices and guidelines is essential to delivering safe and effective care.
Whether you’re looking for information about your education requirements, online learning, immunisation event recordings and presentations, the WA Health Immunisation Education webpage is your go-to resource.
Why check in regularly?
- New events are added throughout the year
- Topics cover clinical updates, vaccine safety, cold chain management, and more
- Opportunities for networking and peer learning
Your commitment to ongoing immunisation education helps keep our communities safe and healthy.
Webinar recordings for NCIRS
The National Centre for Immunisation Research and Surveillance (NCIRS) has concluded a year of insightful, informative webinars that are now all available to watch on demand.
- Australian RSV immunisation Update
- Triple Protection: Vaccines for Influenza, COVID-19 and RSV in 2025
- Navigating vaccination for the immunocompromised patient
- What’s new in Pneumococcal vaccination
- Protecting adolescents through immunisation
To access these webinar recordings, click here.
Don’t ignore the black puppy: Why small signs of depression deserve big attention

WA Primary Health Alliance (WAPHA) has recently launched the ‘Depression starts small’ consumer campaign, designed to promote help seeking behaviours in those experiencing mild and moderate depression symptoms.
It portrays a young man grappling to understand the nature of his depressive symptoms, which are highlighted by an omnipresent black puppy. Watch the Depression starts small hero video. The campaign’s dedicated website has further information and resources for people to delve into.
While many communities across WA will see and benefit from this campaign, we have focused special attention on two population groups and six locations where we have identified that people are at greater risk of poorer health outcomes generally. The target audiences are youth and men in the Swan, Armadale, Goldfields, Bunbury, Manjimup, Goldfields and Esperance regions.
We encourage your practice to promote the campaign to spread further awareness through content that best suits your style and audience via our downloadable campaign supporter kit.
As a result of the campaign, some of your patients may bring up symptoms that they feel are linked to depression. To support the care you provide, you may wish to alert patients to the Medicare Mental Health website where they can find resources for understanding and managing what they’re experiencing.
GPs can refer into Medicare Mental Health by calling 1800 595 212 and the intake clinician can organise to call the patient at a time that suits them to complete the assessment. Alternatively, your patient is welcome to call 1800 595 212 themselves. Clinician Assist WA also has useful pathways for depression.
Free accredited training in disaster preparedness for general practice
Presented by WA Primary Health Alliance
Ongoing e-learning training
Western Australia faces recurring bush fires, floods and other natural disasters, and GPs are the local health professionals working in the community before disasters strike and remain after responders leave.
Provided at no cost to the practice, “Building capacity in disaster preparedness and response for general practice” is a bespoke, accredited* online learning package from WAPHA designed to equip GPs, and practice teams to manage patient flow, prioritise resources, and maintain continuity of care, particularly for those with chronic conditions and mental health needs.
Taking approximately 12 hours to complete (at your own pace), with modules tailored to specific roles within the practice team, participants will learn:
- Practical strategies for disaster preparedness, response, and recovery in primary care
- Maintaining continuity of care and managing patient demand during crises
- Resource prioritisation and supporting priority populations
- Coordinating with local health districts, emergency services and public health agencies
- Building practice resilience, safety systems and structured disaster management processes.
*RACGP Accredited for 11.5 hours (6 EA, 3 RP and 2.5 MO).
Medico-legal considerations for GPs responding to family and domestic violence
Presented by WA Primary Health Alliance
29 November 2025 (8am to 10.30am) Aloft Rivervale – 1.5 RACGP EA hours
This WA Primary Health Alliance workshop invites GPs and supporting members of the practice team to strengthen their response to patients experiencing family and domestic violence (FDV) through best-practice documentation and collaborative care. A multidisciplinary panel from the Sexual Assault Resource Centre, MDA National, Women’s Legal Service and the Police FDV Response Team will share insights on medical and legal processes in responding to FDV.
Download the flyer or register here. Breakfast provided.
Other Webinars, Events & Workshops
Acknowledgement
WA Primary Health Alliance acknowledges and pays respect to the Traditional Owners and Elders of this country and recognises the significant importance of their cultural heritage, values and beliefs and how these contribute to the positive health and wellbeing of the whole community.